
Breasts are made up of fibrous tissue (or connective tissue), glandular tissue (the type of tissue that produces milk), and fatty tissue. Breast cancer is a cancer of the breast tissue. It arises from the uncontrollable cell growth of cells in the breast.
Breast cancer can be categorised in several ways. Most often it is classified by where it originates and whether it moves from that spot.
For prediction of patient prognosis and treatment plan, breast cancer has been clinically staged based on:
Breast cancer is also divided into different molecular subtypes according to the biological characteristics of tumour cells, including:
Biological characteristics of tumour cells have also been included in medical evaluation to select targeted therapies.
Types of breast cancer
Non-invasive breast cancer develops in the cells of a duct or lobule and remains in that location.
Invasive breast cancer develops in the cells of a duct or lobule, but it does not remain where it originated. Instead, it spreads and invades surrounding tissue.
Triple-negative breast cancer (TNBC) is a type of cancer that lacks the expression of three breast cancer cell receptors (Oestrogen Receptor, Progesterone Receptor, and Human Epidermal Growth Factor Receptor Type II or HER-2).
TNBC accounts for about 10% of all breast cancer types in the world. The other 70% are hormone receptor-positive breast cancers and 20% are HER-2 positive breast cancers.
TNBC is regarded as the most difficult type of breast cancer to treat because the cancer cells metastasize more easily to other organs.
Can men get breast cancer?
Although it is rare, men can and do get breast cancer. Men’s breasts are not fully developed like women’s do, but all men have breast tissue.
Signs and symptoms of breast cancer
The symptoms of breast cancer can vary widely and some types of breast cancer may not have any noticeable symptoms.
Some warning signs of breast cancer are:
Keep in mind that these symptoms can happen with other conditions that are not cancer. If you have any signs or symptoms that worry you, be sure to see your doctor right away.
Risk factors of breast cancer
Women with dense breasts have more fibrous and glandular tissues and less fatty tissue in their breasts. They have a higher risk of breast cancer than women with fatty breasts, and the risk increases with increasing breast density.
Triple-negative breast cancer (TNBC) afflicts mostly women who are relatively young (in their 30s or 40s). On the other hand, carriers of the breast cancer genes 1 and 2 (BRCA 1 and BRCA 2) mutations are also more likely to develop TNBC. About 70% of patients with mutated BRCA genes have TNBC.
Diagnosis of breast cancer
Learn more about the different types of screening and diagnostic procedures performed to diagnose breast cancer.
Treatment options for breast cancer
Treatment for breast cancer depends on how big the tumour is and how far it has spread, it may include:
Treatment for triple-negative breast cancer (TNBC)
Triple-negative breast cancer (TNBC) has been regarded as a difficult breast cancer to treat. For a long time, patients with metastatic TNBC can only receive traditional chemotherapy. However, the effect is not significant.
Tumour cells cleverly hide themselves in the human body. Therefore, traditional chemotherapy kills all cells, good or bad. Nowadays, the combination of immunotherapy and chemotherapy is performed to extend the overall survival of patients with metastatic TNBC while reducing the risk of cancer progression.
Chemotherapy first polishes off the surface of the tumour, removes its immune-protective layer and exposes it, thereby assisting the body’s immune cells to recognise cancer cells and launch targeted attacks.
However, TNBC patients must meet one condition for immunotherapy: their tumour cells need to contain more than 1% PD-L1 ligand for immunotherapy to be effective.
Immunotherapy drug Atezolizumab specifically binds to PD-L1 to inhibit its interaction with the PD-1 receptor. The drug activates the patient’s own immune system to recognise and attack tumour cells.
Immunotherapy has less side effects than targeted therapy and chemotherapy. However, immunotherapy has to be combined with chemotherapy, so patients may still experience common side effects of chemotherapy, such as hair loss, nausea, loss of appetite, and fatigue.
The side effects of immunotherapy are usually weaker than those of targeted therapy and chemotherapy. However, immunology is rather complicated because every patient’s immune response is different. Immunotherapy may still cause some side effects or immune-related inflammation such as fever, asthma, and cough, or pneumonia, etc. This is because in the process of stimulating the immune system to recognise tumour cells, the immune response will become more active, and will sometimes attack healthy cells if it is not controlled.
Currently, immunotherapy is administered by intravenous injection. Patients do not need to be hospitalised, but the number of visits to the hospital will be more frequent. Although immunotherapy still does not cure cancer, it can prolong the survival rate. Therefore, patients with triple-negative breast cancer should not be disappointed. As long as there is a glimmer of hope, they should actively cooperate with treatment, and at the same time look forward to more effective therapies or drugs in the future.
Learn more about the different types treatment technologies to treat breast cancer.
Prevention of breast cancer
We highly recommend following all healthy lifestyle practices to reduce the risk of breast cancer:
Detect to Protect!
Early detection is key. Regular breast self-examinations, and mammograms help detect breast cancer in its early stages. Finding breast cancer that has not yet spread gives you the best chance of remaining healthy and cancer-free for many years.
Women should do a breast self-examination regularly from the age of 20 years old. Learn from your nurse or doctor the right way of doing breast self-examination. If you notice any lump at your breast, please consult your doctor.
How to do breast self-examination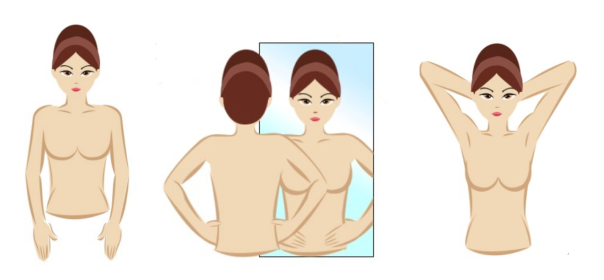

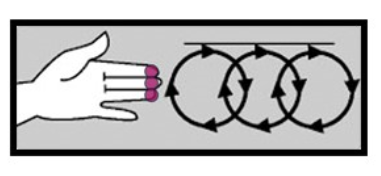
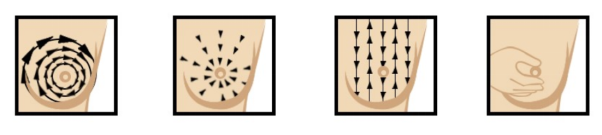
If you notice any lump at your breast or if you are unsure about it, please consult your doctor for a clinical breast examination.
A mammogram is an x-ray of the breast. It can detect breast cancer up to two years before the tumour can be felt by you or your doctor. It is recommended to have a mammogram done every year after age 40.
How does mammography screen for breast cancer?
A breast ultrasound creates computer images of the insides of the breast using sound waves and their echoes. It can reveal some breast changes that may be more difficult to be observed on mammograms, such as fluid-filled cysts.
How does an ultrasound screen for breast cancer?
A breast biopsy may be required if symptoms or the findings of an imaging test (such a mammogram) indicate the possibility of breast cancer. Small samples of breast tissue are taken from the suspicious region during a biopsy so they may be tested in a lab.
How does a biopsy screen for breast cancer?
Make an appointment at Gleneagles Hospitals
While a diagnosis of breast cancer can be overwhelming, the good news is that treatments are available and the rate of successful recovery has increased in recent years.
If you or someone in your family is facing any breast cancer symptoms, get in touch with us to find out more about our Oncology Services at your nearest Gleneagles Hospital.
Gleneagles Hospital works with oncologists to assist patients through cancer treatment. The caring and multidisciplinary team of healthcare professionals are available for consultation and to provide the best care.

Wait a minute

Wait a minute