COVID-19 - Vaccine
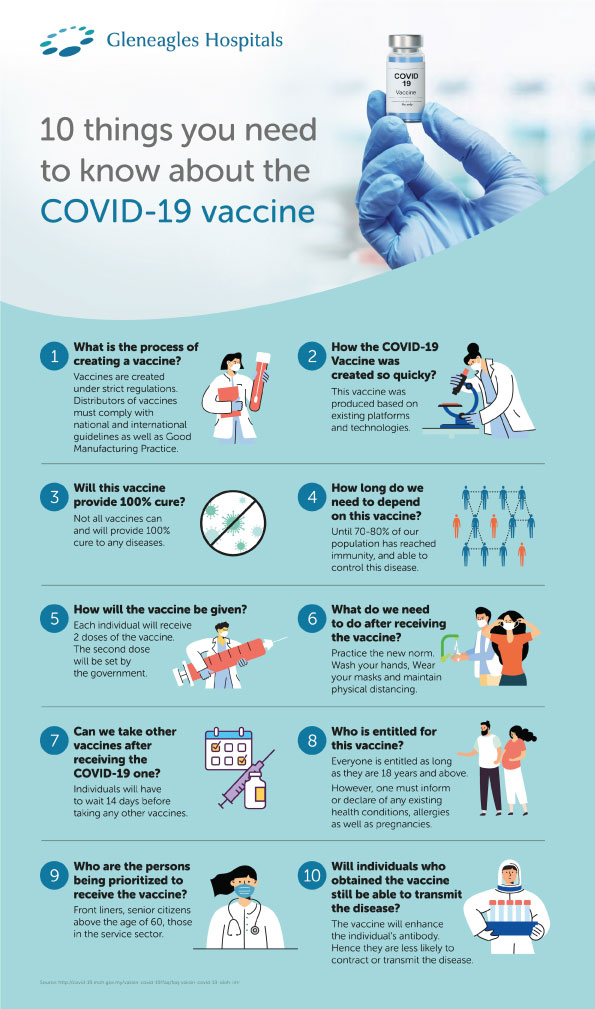
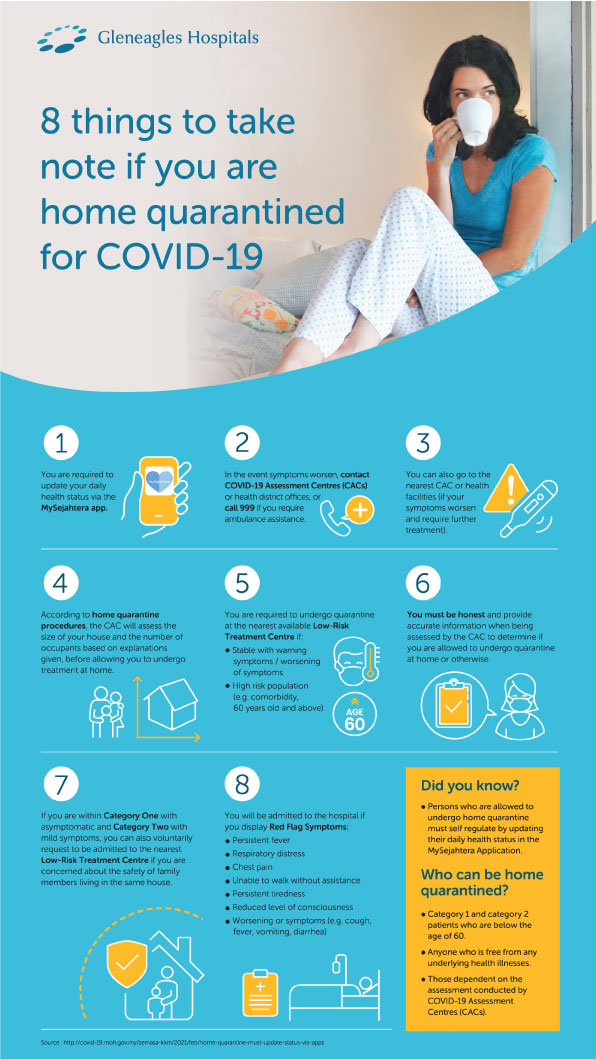
What is the COVID-19 vaccine?
COVID-19 vaccine helps our bodies develop immunity against COVID-19 virus by stimulating our immune system to fight SARSCoV-2 (severe acute respiratory syndrome coronavirus 2) whenever we are exposed to it.
Various platforms such as RNA genetic sequencing, viral vectors, deactivating viruses and protein sub-units have been used to provide safe and effective coronavirus vaccines. It gives you the best protection against COVID-19.
The COVID-19 vaccine is regulated and complies with the following Acts:
- Poisons Act 1952 (Act 366) and its regulations
- Sale of Drugs Act 1952 (Act 368) and its regulations
- Drugs and Cosmetic Control Regulations 1984
- Infectious Disease Prevention and Control Act (Act 342)
Studies have shown that getting vaccinated against COVID-19 can lower your risk of getting and spreading the virus that causes COVID-19. Vaccines also help reduce the risk of severe illnesses and deaths from COVID-19 infections among people who are fully vaccinated.
Getting sick with COVID-19 can cause serious health consequences, even in children. Currently, there are no reliable ways to predict who will have mild or severe illness or who may have long-term health issues after COVID-19 infection.
Therefore, do ensure that you and your family are fully vaccinated. Take your booster doses when you are eligible and consider enrolling your children for vaccination once it is available to them.
Understanding COVID-19 Vaccines
At the moment, frontrunners in the coronavirus vaccine race include Moderna, Pfizer BioNTech, Sinovac Biotech and Oxford AstraZeneca.
The vaccines protect against symptomatic forms of COVID-19, but it is still unclear whether they will stop the spread of the SARS-CoV-2 virus, the cause of COVID-19. Therefore, you should still continue to take appropriate precautions in protecting yourself and others around you even after receiving the COVID-19 vaccine.
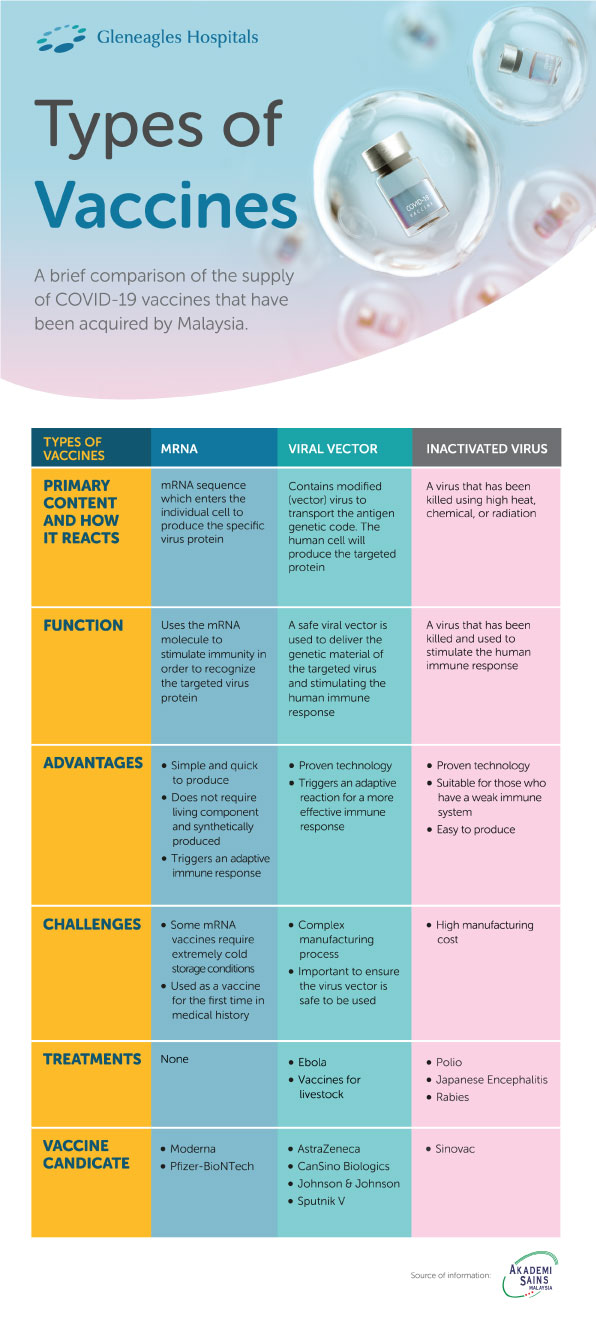
| Types of vaccines | mRNA | Viral vector | Inactivated virus |
|---|---|---|---|
Primary Content And How It
Reacts
| mRNA sequence which enters the individual cell to produce the specific virus protein | Contains modified (vector) virus to transport the antigen genetic code. The human cell will produce the targeted protein | A virus that has been killed using high heat, chemical, or radiation |
Function
| Uses the mRNA molecule to stimulate immunity in order to recognize the targeted virus protein | A safe viral vector is used to deliver the genetic material of the targeted virus and stimulating the human immune response | A virus that has been killed and used to stimulate the human immune response |
Advantages
|
|
|
|
Challenges
|
|
|
|
Treatments
| None |
|
|
Vaccine Candidate
|
|
|
|
Source of information: AKADEMI SAINS MALAYSIA
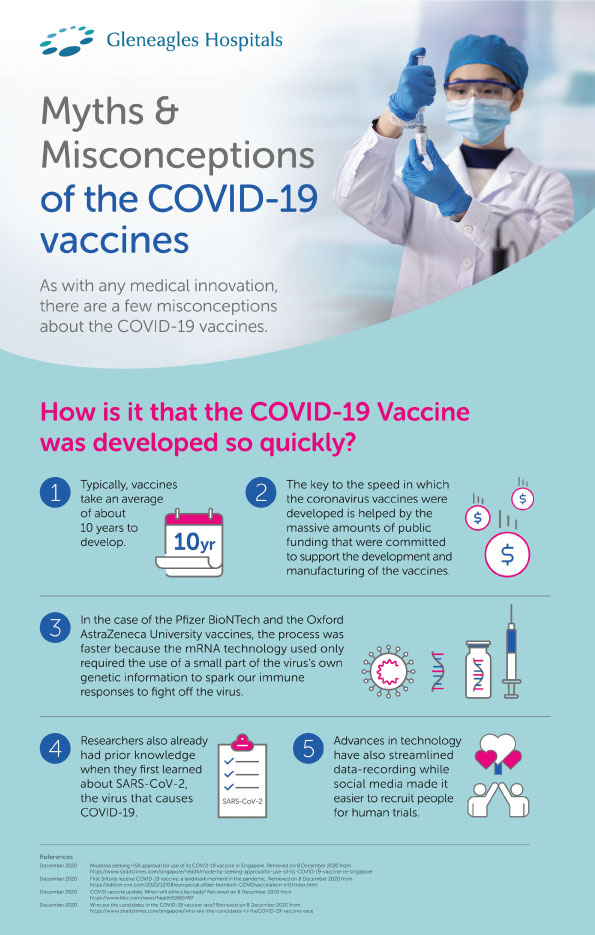
- Technology and the COVID-19 vaccine
Both the Moderna and Pfizer BioNTech’s vaccines use mRNA (messenger RNA) technology and it is interesting to note that the mRNA vaccines have never been approved for use in any disease. It has however received emergency use authorization from the FDA.
mRNA vaccines work by injecting pieces of the virus’ genetic code into the body to stimulate an immune system reaction which enables the body to defend itself against the coronavirus.
The mRNA in the body breaks down fully within 48 hours. As it doesn’t enter the human nucleus, it does not affect human DNA. Both Moderna and Pfizer’s mRNA vaccines require 2 doses for adequate protection, and the doses are administered between 3 and 4 weeks apart.
Oxford AstraZeneca and Sinovac Biotech’s vaccines employ a modified delivery virus (that usually causes symptoms such as the common cold) to introduce SARS-CoV-2 viral proteins to the immune system, which then mounts a defence against it. The delivery virus is attenuated or modified so the person won’t develop the common cold when administered with this vaccine.
Why is COVID-19 vaccination important?
The national COVID-19 immunisation programme by the Malaysian government is an important step to stop the pandemic. Benefits from the immunisation programme include;
- Preventing someone from COVID-19 infection or becoming seriously ill due to COVID-19.
- Curb the spread of COVID-19 to others.
- To achieve herd immunity where a significant amount of the population is protected through vaccination against the virus, making it difficult for the disease to spread.
- Infectious Disease Prevention and Control Act (Act 342)
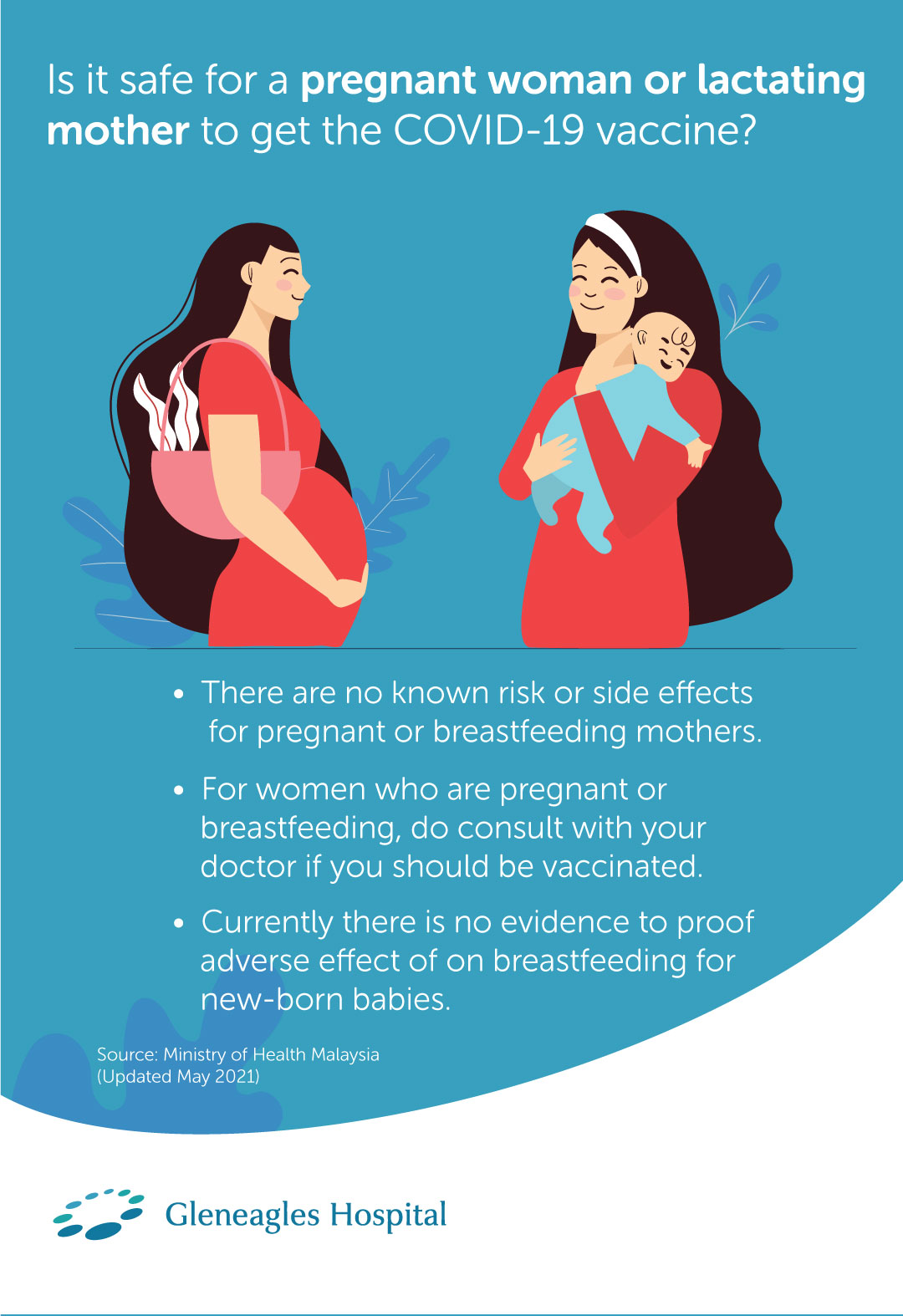
COVID-19 Vaccination – Safe for
Pregnant Women and Breastfeeding Mothers?
Update: Recent announcement by the Ministry of Health, Malaysia on 25 May 2021 indicated that only the Pfizer vaccine is allowed for pregnant women between week 14 and 33, or they should defer vaccination till after their delivery. The AstraZeneca and Sinovac vaccines are not recommended at the moment. As for breastfeeding mothers, both the Pfizer and AstraZeneca vaccines are suitable for them. For Sinovac vaccine, it is currently not recommended for pregnant women due to the limited clinical data. Breastfeeding mothers who would like to opt for Sinovac vaccine are required to consult their specialists prior to vaccination.
| Vaccine | Pregnant Mothers | Lactating Mothers |
|---|---|---|
Pfizer
| Suitable for pregnant mothers between 14 – 33 weeks of pregnancy. Or delay until after delivery. | Suitable to be vaccinated. |
Astra Zeneca
| Not recommended at the moment. | Suitable to be vaccinated. |
Sinovac
| Not recommended at the moment. | Limited clinical data. Recommendation will be given after consultation. |
Source of information: Kementerian Kesihatan Malaysia
Government bodies and health authorities around world are encouraging
eligible members of the general public to get vaccinated. This is
because as more people get vaccinated it reduces the chances of
transmission.
Which means it becomes more difficult for the virus to spread, hence
making it safer for the society if more people get vaccinated.
But, what if you are pregnant or breastfeeding? Is it (really)
safe to get vaccinated for COVID-19?
Is it safe to get vaccinated if you are
pregnant?
There is currently very little data available to assess the
safety of COVID -19 vaccines on pregnant women and breastfeeding
mothers because of the lack of clinical testing during the
development
of the COVID-19 vaccine. Having said that, based on the safety and
efficacy data of the current vaccines in the market, the World
Health Organization (WHO) states they do not have any reason to
believe
there will be specific risks that would outweigh the benefits of
vaccination for pregnant women. In fact, findings of a few studies
did not indicate any adverse effects on fetal development.
Additionally, pregnant women and breastfeeding mothers
have also taken other vaccines such as tetanus toxoid, influenza and
pertussis for example. However, If you are still unsure, we highly
recommend that you speak to your OB-GYN to seek advice and discuss
about your eligibility for COVID -19 vaccination.
Is it safe to get vaccinated if you are
breastfeeding?
While there is currently very little data to suggest the
safety and efficacy of the COVID -19 vaccines on pregnant women or
breastfeeding mothers, there are also no known risks of the COVID-19
vaccine to breastfeeding mothers.
This is because the vaccines currently available in the market
are non-replicating vaccines. Non-replicating vaccines can create an
immune response but do not reproduce inside host cells –
meaning that there is no possible way by which the vaccine can pass
to your baby through breast milk.
- It is encouraged for pregnant woman and breastfeeding mother to consider getting vaccinated against COVID -19 especially if you are in the frontline e.g. a healthcare worker or have known medical conditions. However, the decision should be made as a mutual agreement between the mother and her consultant. She should get clearance from her consultant prior to considering getting vaccinated for COVID-19.
- Despite insufficient data on the potential effects of the Covid-19 vaccines in expecting and nursing mothers, the Health Ministry will allow them to be inoculated if the benefits outweigh the risks. However, the decision to either allow or advise these mothers against receiving their vaccine shots must come from a specialist after assessing their potential risk
One of the key considerations to note is that women who are pregnant and part of a group recommended to receive the Covid-19 vaccine, such as healthcare personnel, may choose to be vaccinated after thorough discussions with their doctor.
ReferencesSource: Ministry of Health Malaysia (Updated February 2021) World
Health Organization (WHO) (Updated February 2021)
“Panduan Vaksinasi Untuk Ibu Mengandung dan Ibu
Menyusukan Bayi”. Kementerian Kesihatan Malaysia.
Accessed from
http://covid-19.moh.gov.my/vaksin-covid-19/panduan/panduan-vaksinasi-untuk-ibu-mengandung-dan-ibu-menyusukan-bayi
COVID-19 Vaccine – Safe for those with
heart conditions?
Can those with cardiovascular conditions or heart problems
take the
COVID-19 vaccine?
In short, yes. In fact, heart patients are highly encouraged
to take the COVID-19 vaccine as it can help to protect them from
contracting the virus. Here’s why.
According to studies, heart patients have a higher risk
of developing health complications from COVID-19 compared to those
without history of heart problems. That is why, heart patients fall
under a group of people who have been prioritized to get the
COVID-19 vaccine alongside other patients with chronic diseases such
as diabetes, hypertension and high cholesterol etc.
Therefore, if you are an individual that have heart
conditions, or if your family member is a heart patient, you should
take or advice your family member to get vaccinated against COVID-19
– by taking this action, not only are you protecting yourself
but you are also protecting your loved ones from COVID-19.
However, it is understood that you may have some
concerns over the safety of the COVID-19 vaccine, especially since
you or your loved ones have pre-existing medical conditions. Would
it worsen
the condition or will the side-effects be more severe?
Will those with cardiovascular disease or heart
problems
experience
any side effects?
The current mRNA COVID-19 vaccines available in the market
have been shown to be safe for use for heart patients. This is
because people with pre-existing medical conditions such as
diabetes, heart
problems, hypertension and high cholesterols were included in the
early clinical trials.Which means that the vaccines have been tried
and tested by people who have the same medical conditions as you
and they were found to benefit from the vaccine.
When it comes to side effects, most vaccine can have
side effects. It is important to note that both the mRNA vaccines
PfizerBioNTech and Moderna do carry the risk of some common side
effects
such as pain, redness or swelling in the shoulder muscle area where
the injections were administered, as well as fatigue, headaches,
muscle pain, chills, fever and nausea. These symptoms will most
likely
resolve within one or two days. If the symptoms persist, please
consult a healthcare professional for medical advice.
However, if you history of allergic reaction to any
component (active ingredients or excipients or any material used in
process) of the vaccine or similar vaccines, it is advisable for you
not to get the vaccine – not at least until more safety data
become available.
Should you get vaccinated if you have
cardiovascular disease
or heart problems?
Yes, you should. As advised by Ministry of Health, everyone
who is medically eligible should get vaccinated. This is because as
more people get vaccinated, the slower the virus would spread, and
as a result our community will be safer.
However, if you are still concerned about the safety of
these vaccinations, we encouraged you to seek consultation with your
doctor. Click here to speak with our doctors. Our doctors will
be able to assess your medical and allergy history to determine your
eligibility for COVID-19 vaccines.
However, if you still have concerns, you may well get
advice from your consultant.
References
1. “Should heart patients take the COVID-19 vaccine?”.
Singapore Heart Foundation.
Accessed from
https://www.myheart.org.sg/press-and-media/heart-news/heart-patient-and-covid19-vaccine/
2. “The effects of virus variants on COVID-19
vaccines”. World Health Organization (1 March 2021).
Accessed from
https://www.who.int/news-room/feature-stories/detail/the-effects-of-virus-variants-on-COVID-19-vaccines
3. Merschel, M. “What heart and stroke patients should
know about COVID-19 vaccines”. The American Heart Association.
Accessed from
https://www.heart.org/en/news/2021/01/15/what-heart-and-stroke-patients-should-know-about-COVID-19-vaccines
4. “COVID-19 VACCINATION”. Ministry of Health
Singapore (n.d).
Accessed from
https://www.moh.gov.sg/COVID-19/vaccination
None of us ever expected that our lives would change indefinitely
when the COVID-19 pandemic took over the entire world by storm. We
are now left to embrace the ‘new normal’ of living.
Something
that still needs getting used to. Some light did come to show early
this year when some pharmaceutical companies begun rolling out the
much-awaited COVID-19 vaccine. Even so, they are increasing the
production of these vaccines as we progress daily.
This is a step in the right direction as it prepares us
to return to normal life by achieving herd immunity – a term
used to describe a huge population that is immune to a virus.
Through
herd immunity, the risk of large-scale outbreaks – like we
have seen over the past year – is significantly reduced1.
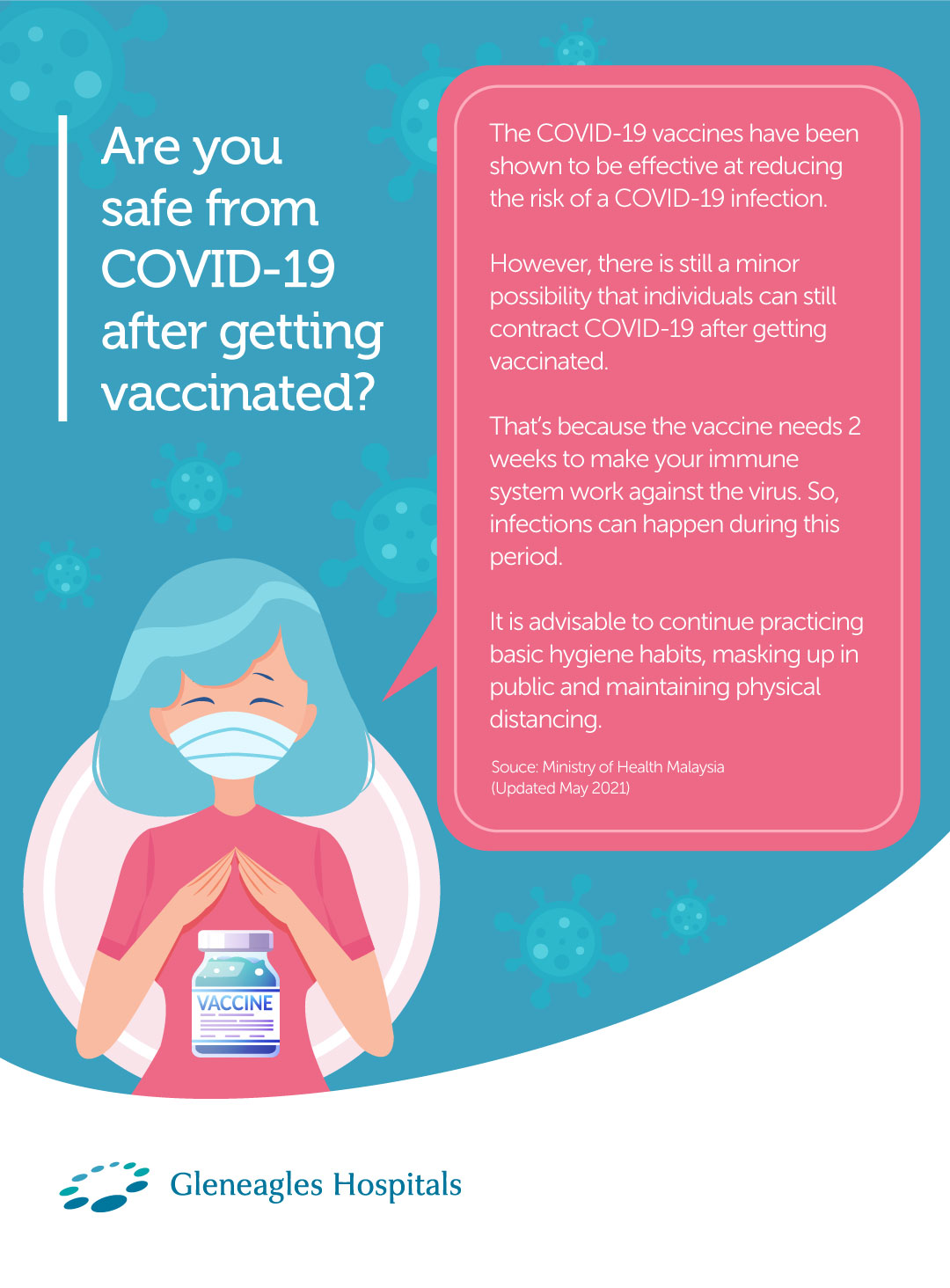
However, two important questions remain – can you still get
infected
with COVID-19 after taking the vaccine, and are you eligible for the
vaccine if you have previously tested positive for the virus?
Let’s find out together.
Can those who get vaccinated still contract
COVID-19?
Let us first understand that the COVID-19 vaccines that were
developed have been found to be effective at preventing a COVID-19
infection. However, there is still a minor possibility that you can
contract
COVID-19 despite being vaccinated. Rest assured, that it is a very
slim chance and with vaccination already taking place at break
speed, the risk of COVID-19 infections become even lower.
It’s also important to be aware that the
coronavirus vaccine might not have enough time to provide complete
protection - not that it is ineffective against COVID-19. This is
why mRNA
vaccinations need to be given in two dosages and require
approximately two weeks to fully activate our immune system
response.
So even if an individual has received the vaccination,
practicing cautions in social or physical distancing as well as
basic hygiene is crucial.
Can those who have been previously diagnosed
with COVID-19 be vaccinated?
A person can take the vaccine until the person has recovered from the
acute illness (if the person had symptoms) and they have met
criteria to discontinue isolation. Why? Getting vaccinated can offer
a stronger
and reliable immune system response to a past COVID-19 infection as
compared to the natural immunity developed by the body.
As a matter of fact, those who have recovered from
COVID-19 were found to have antibodies that were up to 10 times
higher than vaccinated individuals who did not previously test
positive
for COVID-19. But those with pre-existing immunity experienced
systemic side effects such as fatigue, headache, chills, fever, and
muscle or joint pains with considerably higher frequency This is why
those who fall in this category are also encouraged to sign-up for
vaccination as soon as possible.
Will life return to normal for those who
have been vaccinated?
Hopefully it will. The most important thing is to do your duty as a good citizen by signing up for the vaccination. However, getting vaccinated against COVID-19 should not be considered a substitute for basic precautionary measures. We should always remember to do our part by practicing good hygiene habits like regular hand-washing, masking up when outdoors, and adhering to social distancing measures. By doing this, we are one step closer to beating the pandemic once and for all.
References
1. “Coronavirus disease (COVID-19): Vaccines”. World
Health Organization (28 October 2020).
Accessed from
https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines
2. “Information about the Pfizer-BioNTech COVID-19
Vaccine”. Centers for Disease Control and Prevention (4 March
2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Pfizer-BioNTech.html
3. “Information about the Moderna COVID-19
Vaccine”. Centers for Disease Control and Prevention (4 March
2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Moderna.html
4. “Key Things to Know About COVID-19 Vaccines”.
Centers for Disease Control and Prevention (13 March 2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/keythingstoknow.html
5. Wise, J. “Covid-19: People who have had infection
might only need one dose of mRNA vaccine”. thebmj (2 February
2021).
Accessed from
https://www.bmj.com/content/372/bmj.n308
Studies have shown that it is natural for any type of virus to evolve
into newer variants. It simply means that viruses can mutate after
some time. This doesn’t mean that they are a new form of a
virus,
but rather a different kind of the same virus.
Best way to describe this is is to think of them as
being part of the same family. Now, these new strains may cause some
changes that are a little different from how we understand the
original
virus to be. While many would panic especially when we keep hearing
about the COVID-19 new variants, its best we first understand how
this mutation works.
It’s true, new strains can either increase or
decrease the risk of a virus being contagious. These strains may
also affect the severity or level of an infection. So, in the case
of
COVID-19, how exactly do new strains affect the level of symptoms?
Does it impact the effectiveness of the different vaccines that are
already available? Let’s take a closer look at how these
happens.
Can a new virus strain cause more severe
COVID-19 symptoms?
Before we dive in a little deeper, it’s important to note that
virus strains exist because of differences in geographic location.
What does that mean, you ask? It means that different countries or
regions may have the same primary virus, but new and different virus
strains may appear in these places simply because of geographical
reasons Let’s look at the virus strain that was originally
detected in the UK for example. This virus strain, also known as
B117, was found to increase the risk of being contagious by up to
50% compared to the original COVID-19 virus. Whoa!
The South African strain - B1351 - on the other hand,
was found to be 50% more contagious than the original COVID-19
virus3. Similarly, the P1 virus strain that was first detected in
Brazil
was found to be up to 2.2 times more contagious than the B117
variant. Pretty intense we would say, but does a higher risk of
being contagious mean that there are more severe COVID-19 symptoms?
Meanwhile, B117 (UK) and B1351 (South Africa) have not
been found to affect the level of COVID-19 symptoms experienced.
However, more data is required to understand the level of COVID-19
symptoms experienced by those infected with the P1 (Brazil) strain.
More recently is the strain discovered out of India
(B.1.617) which has caused global record numbers in daily infections
within the country over the past weeks. It’s still too early
to say if this strain is the cause of rapid spread in India, but
experts are treating it as such. It’s also being called a
“super mutation” that will make its way around to the
rest
of the world. Oh no! This strain has already been detected in
countries like Germany, Belgium and even in the U.K.
This is why it’s important to continue practicing
basic precautionary measures and get vaccinated as soon as possible.
Through this, you are doing your civic duty as a responsible citizen
to prevent further widespread of these new strains.
Can a new virus strain affect the
effectiveness of the different vaccines available?
According to the World Health Organisation (WHO), there is no reason
to believe that these COVID-19 virus strains can cause any vaccine
to be ineffective We can totally breathe easy now! This is because
COVID-19 vaccinations give our bodies some sort of protection by
working with our immune system, which is the body’s natural
defense against viral infections. Through this, our bodies’
natural
defenses cover a wide range of COVID-19 infections, even the new
variants.
On a brighter note, it’s also possible to make
changes to existing vaccines so that they offer better protection
against different COVID-19 virus strains1. This will be especially
important
if data ever shows that these new strains cause the COVID-19
vaccines to be not effective, however there is no such news yet. We
know, what a relief!
What can you do to prevent COVID-19 virus
strains?
Ultimately, it’s important for you to get vaccinated as soon as possible to prevent a COVID-19 infection. And by keeping the spread of the primary virus low, you help to reduce the risk of creating new virus strains in your country or region. Pretty simple, no? At the same time, it’s recommended that you carry on practicing basic measures such as regular hand-washing, masking up, and maintaining social distancing in public areas. By doing this, you can help to reduce the contagiousness of the main COVID-19 virus, whilst reducing the risk of COVID-19 virus strains altogether1. You’ve got this, people!
References
1. “The effects of virus variants on COVID-19 vaccines”.
World Health Organization (01 March 2021).
Accessed from
https://www.who.int/news-room/feature-stories/detail/the-effects-of-virus-variants-on-covid-19-vaccines
2. “Pfizer-BioNTech COVID-19 Vaccine Overview and
Safety”. Centers for Disease Control and Prevention (21 May
2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Pfizer-BioNTech.html
3. CJuan C. Salazar, MD, MPH, FAAP.“What Are the New
COVID-19 Strains, and Do They Infect Kids More Easily?”. (01
February 2021).
Accessed from
https://www.connecticutchildrens.org/coronavirus/what-is-the-new-b117-strain-of-covid-19-and-does-it-more-easily-infect-kids/
4. Simon Clarke.“Brazil coronavirus variant: what is it
and why is it a concern? An expert explains”. (03 March 2021).
Accessed from
https://theconversation.com/brazil-coronavirus-variant-what-is-it-and-why-is-it-a-concern-an-expert-explains-156234
5. “New COVID variant with 5 mutations identified in
California”. Center for Infectious Disease Research and Policy
(12 February 2021).
Accessed from
https://www.cidrap.umn.edu/news-perspective/2021/02/new-covid-variant-5-mutations-identified-california
6. David Kennedy.“What you need to know about the new
COVID-19 variants”. (16 January 2021).
Accessed from
https://theconversation.com/what-you-need-to-know-about-the-new-covid-19-variants-153366
7. “SARS-CoV-2 Variant Classifications and
Definitions”. Center for Infectious Disease Research and
Policy (25 May 2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/variant-surveillance/variant-info.html
8. Gayathri Vaidyanathan. “Coronavirus variants are
spreading in India — what scientists know so far”. (11
May 2021).
Accessed from
https://www.nature.com/articles/d41586-021-01274-7
A visit to the doctor’s for orthopedic problems (joints, ligaments, tendons, muscles, and nerves) during a pandemic can be an uneasy experience. But it sure can be rewarding if you’re heading there for a COVID-19 shot. Why, you ask? If you have any type of pre-existing health condition, you may be at higher risk of getting COVID-19 than someone else without them. Simple equation!
Therefore, it's important to consider getting vaccinated immediately if you are eligible. But one question could be on your mind: is it safe to give the COVID-19 vaccine to someone who is going for orthopedic surgery? Let’s deep dive together to answer this question, shall we?
Is it safe for those undergoing orthopedic
surgery to take the COVID-19 vaccine?
It's generally safe for you to take the COVID-19 vaccine if you are considered eligible. However, if you are undergoing surgery, you should first consult a doctor before getting vaccinated. Chances are that the doctor will advise you not to take it before surgery.
This is because any side effect from the vaccine may impact the outcome of the surgery. For example, any common side effect such as fever or muscle ache may slow down the rehabilitation or prolong the duration of hospitalization. On the other hand, patients who have experienced physical trauma (fractures, broken or dislocated bones) due to a car accident, fall or sports injury, may be asked upon arrival at the Emergency department if they already have received the COVID-19 vaccination.
Those who have bone or blood-related diseases (bone cancer, osteoporosis, and leukemia) that are severe and can cause terminal illness should also seek consultation with a doctor before getting the COVID-19 vaccine. Better to be safe than sorry, people.
Is it safe to take the COVID-19 vaccine
alongside pain management medicine prior to surgery?
Yes, it is safe for someone who has been given pain management medicine such as steroids for joint pain or inflammation to get the COVID-19 vaccine2. Also, it’s recommended to consult with the clinician in charge for medical advice.
This piece of good news will make no one happier than the elderly. Why the elderly, you may ask? Well, for one, old age can put a person at a bigger risk of injury or developing orthopedic conditions 3. For example, arthritis, which requires medicine to manage the pain caused by swollen or tender joints. Ouch!
At the same time, old age can also lower immune system function (your body’s natural defenses) and increase the risk of infectious diseases like COVID-194. This is why it’s important for the elderly to prioritise getting vaccinated, as it can help to protect them against the harmful effects of COVID-194.
If you’re not sure about taking the COVID-19 vaccine while on steroid treatment, we encourage you to speak to our orthopedic specialists and come to a decision that works best for you.
Should you get vaccinated prior to
orthopedic surgery?
Yes. But before you do, we recommend that you speak to any of our doctors. They’re best qualified to decide if you are eligible for the COVID-19 vaccine, or if you’re at risk of having health problems due to vaccination. The doctor’s decision to not allow you to take the vaccine relies on things like a weakened immune system, a platelet count that is less than 50,000, and a history of experiencing a severe allergic reaction (also known as anaphylaxis) to venom, certain foods or medication5.
In parting, just remember, It takes a joint (pun intended) effort by everyone to achieve complete immunity within our communities. This starts with prioritising vaccination and other preventive measures such as regular handwashing, masking up in public places, and maintaining social distancing.
References1. Blouhos, K, et al. “Understanding Surgical Risk During
COVID-19 Pandemic: The Rationale Behind the Decisions”.
Frontiers in Surgery.
Accessed from
https://www.frontiersin.org/articles/10.3389/fsurg.2020.00033/full
2. Chakarvarty, K, et al. “Recommendations and Guidance
for Steroid Injection Therapy and COVID-19 Vaccine Administration
from the American Society of Pain and Neuroscience (ASPN)”.
Dovepress (5 March 2021). Centers for Disease Control and Prevention
(21 May 2021).
Accessed from
https://www.dovepress.com/recommendations-and-guidance-for-steroid-injection-therapy-and-covid-1-peer-reviewed-fulltext-article-JPR
3. Anderson, A. S, MD and Loeser, F. R, MD. “Why is
Osteoarthritis an Age-Related Disease?”. US National Library
of Medicine (24 February 2010).
Accessed from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2818253/
4. “Aging changes in immunity”. MedlinePlus.
Accessed from
https://medlineplus.gov/ency/article/004008.htm
5. “COVID-19 VACCINATION”. Ministry of Health
Singapore (n.d).
Accessed from
https://www.moh.gov.sg/covid-19/vaccination
6. “Thrombocytopenia following Pfizer and Moderna
SARS-CoV-2 vaccination”. The National Center for Biotechnology
Information.
Accessed from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8014568/

1. What are the types of vaccines?
At the moment, frontrunners in the coronavirus vaccine race include Moderna, Pfizer BioNTech, Sinovac Biotech and Oxford AstraZeneca.
| Types of vaccines | mRNA | Viral vector | Inactivated virus |
|---|---|---|---|
Primary Content And How It
Reacts
| mRNA sequence which enters the individual cell to produce the specific virus protein | Contains modified (vector) virus to transport the antigen genetic code. The human cell will produce the targeted protein | A virus that has been killed using high heat, chemical, or radiation |
Function
| Uses the mRNA molecule to stimulate immunity in order to recognize the targeted virus protein | A safe viral vector is used to deliver the genetic material of the targeted virus and stimulating the human immune response | A virus that has been killed and used to stimulate the human immune response |
Advantages
|
|
|
|
Challenges
|
|
|
|
Treatments
| None |
|
|
Vaccine Candidate
|
|
|
|
Source of information: AKADEMI SAINS MALAYSIA
The vaccines protect against symptomatic forms of COVID-19, but it is still unclear whether they will stop the spread of the SARS-CoV-2 virus, the cause of COVID-19. Therefore, you should still continue to take appropriate precautions in protecting yourself and others around you even after receiving the COVID-19 vaccine.
Technology and the COVID-19 vaccine
Both the Moderna and Pfizer BioNTech’s vaccines use mRNA (messenger RNA) technology and it is interesting to note that the mRNA vaccines have never been approved for use in any disease. It has however received emergency use authorization from the FDA.
mRNA vaccines work by injecting pieces of the virus’ genetic code into the body to stimulate an immune system reaction which enables the body to defend itself against the coronavirus.
The mRNA in the body breaks down fully within 48 hours. As it doesn’t enter the human nucleus, it does not affect human DNA. Both Moderna and Pfizer’s mRNA vaccines require 2 doses for adequate protection, and the doses are administered between 3 and 4 weeks apart.
Oxford AstraZeneca and Sinovac Biotech’s vaccines employ a modified delivery virus (that usually causes symptoms such as the common cold) to introduce SARS-CoV-2 viral proteins to the immune system, which then mounts a defence against it. The delivery virus is attenuated or modified so the person won’t develop the common cold when administered with this vaccine.
2. Why is COVID-19 vaccination important?
Why is COVID-19 vaccination important?
The national COVID-19 immunisation programme by the Malaysian government is an important step to stop the pandemic. Benefits from the immunisation programme include;
- Preventing someone from COVID-19 infection or becoming seriously ill due to COVID-19.
- Curb the spread of COVID-19 to others.
- To achieve herd immunity where a significant amount of the population is protected through vaccination against the virus, making it difficult for the disease to spread.
- Infectious Disease Prevention and Control Act (Act 342)
3. Is it safe for pregnant women and breastfeeding
mothers?
COVID-19 Vaccination – safe for
Pregnant Women and Breastfeeding Mothers?
Update: Recent announcement by the Ministry of
Health, Malaysia on 25 May 2021 indicated that only the Pfizer
vaccine is allowed for pregnant women between week 14 and 33, or
they should
defer vaccination till after their delivery. The AstraZeneca and
Sinovac vaccines are not recommended at the moment. As for
breastfeeding mothers, both the Pfizer and AstraZeneca vaccines are
suitable
for them. For Sinovac vaccine, it is currently not recommended for
pregnant women due to the limited clinical data. Breastfeeding
mothers who would like to opt for Sinovac vaccine are required to
consult
their specialists prior to vaccination.
| Vaccine | Pregnant Mothers | Lactating Mothers |
|---|---|---|
Pfizer
| Suitable for pregnant mothers between 14 – 33 weeks of pregnancy. Or delay until after delivery. | Suitable to be vaccinated. |
Astra
Zeneca
| Not recommended at the moment. | Suitable to be vaccinated. |
Sinovac
| Not recommended at the moment. | Limited clinical data. Recommendation will be given after consultation. |
Source of information: Kementerian Kesihatan Malaysia
Government bodies and health authorities around world are encouraging
eligible members of the general public to get vaccinated. This is
because as more people get vaccinated it reduces the chances of
transmission.
Which means it becomes more difficult for the virus to spread, hence
making it safer for the society if more people get vaccinated.
But, what if you are pregnant or breastfeeding? Is it
(really) safe to get vaccinated for COVID-19?
There is currently very little data available to assess the safety of
COVID -19 vaccines on pregnant women and breastfeeding mothers
because of the lack of clinical testing during the development of
the
COVID-19 vaccine. Having said that, based on the safety and efficacy
data of the current vaccines in the market, the World Health
Organization (WHO) states they do not have any reason to believe
there
will be specific risks that would outweigh the benefits of
vaccination for pregnant women. In fact, findings of a few studies
did not indicate any adverse effects on fetal development.
Additionally, pregnant women and breastfeeding mothers
have also taken other vaccines such as tetanus toxoid, influenza and
pertussis for example. However, If you are still unsure, we highly
recommend that you speak to your OB-GYN to seek advice and discuss
about your eligibility for COVID -19 vaccination.
While there is currently very little data to suggest the safety and
efficacy of the COVID -19 vaccines on pregnant women or
breastfeeding mothers, there are also no known risks of the COVID-19
vaccine to
breastfeeding mothers.
This is because the vaccines currently available in the
market are non-replicating vaccines. Non-replicating vaccines can
create an immune response but do not reproduce inside host cells
– meaning that there is no possible way by which the vaccine
can pass to your baby through breast milk.
- It is encouraged for pregnant woman and breastfeeding mother to consider getting vaccinated against COVID -19 especially if you are in the frontline e.g. a healthcare worker or have known medical conditions. However, the decision should be made as a mutual agreement between the mother and her consultant. She should get clearance from her consultant prior to considering getting vaccinated for COVID-19.
- Despite insufficient data on the potential effects of the Covid-19 vaccines in expecting and nursing mothers, the Health Ministry will allow them to be inoculated if the benefits outweigh the risks. However, the decision to either allow or advise these mothers against receiving their vaccine shots must come from a specialist after assessing their potential risk
One of the key considerations to note is that women who are pregnant and part of a group recommended to receive the Covid-19 vaccine, such as healthcare personnel, may choose to be vaccinated after thorough discussions with their doctor.
References
Source: Ministry of Health Malaysia (Updated February 2021) World
Health Organization (WHO) (Updated February 2021)
“Panduan Vaksinasi Untuk Ibu Mengandung dan Ibu
Menyusukan Bayi”. Kementerian Kesihatan Malaysia.
Accessed from
http://covid-19.moh.gov.my/vaksin-covid-19/panduan/panduan-vaksinasi-untuk-ibu-mengandung-dan-ibu-menyusukan-bayi
4. Is it safe for those with heart conditions?
COVID-19 Vaccine – Safe for those with
heart conditions?
Can those with cardiovascular
conditions or heart problems
take the
COVID-19 vaccine?In short, yes. In fact, heart patients are highly encouraged to take
the COVID-19 vaccine as it can help to protect them from contracting
the virus. Here’s why.
According to studies, heart patients have a higher risk
of developing health complications from COVID-19 compared to those
without history of heart problems. That is why, heart patients fall
under a group of people who have been prioritized to get the
COVID-19 vaccine alongside other patients with chronic diseases such
as diabetes, hypertension and high cholesterol etc.
Therefore, if you are an individual that have heart
conditions, or if your family member is a heart patient, you should
take or advice your family member to get vaccinated against COVID-19
– by taking this action, not only are you protecting yourself
but you are also protecting your loved ones from COVID-19.
However, it is understood that you may have some
concerns over the safety of the COVID-19 vaccine, especially since
you or your loved ones have pre-existing medical conditions. Would
it worsen
the condition or will the side-effects be more severe?
The current mRNA COVID-19 vaccines available in the market have been
shown to be safe for use for heart patients. This is because people
with pre-existing medical conditions such as diabetes, heart
problems,
hypertension and high cholesterols were included in the early
clinical trials.Which means that the vaccines have been tried and
tested by people who have the same medical conditions as you and
they were
found to benefit from the vaccine.
When it comes to side effects, most vaccine can have
side effects. It is important to note that both the mRNA vaccines
PfizerBioNTech and Moderna do carry the risk of some common side
effects
such as pain, redness or swelling in the shoulder muscle area where
the injections were administered, as well as fatigue, headaches,
muscle pain, chills, fever and nausea. These symptoms will most
likely
resolve within one or two days. If the symptoms persist, please
consult a healthcare professional for medical advice.
However, if you history of allergic reaction to any
component (active ingredients or excipients or any material used in
process) of the vaccine or similar vaccines, it is advisable for you
not to get the vaccine – not at least until more safety data
become available.
Yes, you should. As advised by Ministry of Health, everyone who is
medically eligible should get vaccinated. This is because as more
people get vaccinated, the slower the virus would spread, and as a
result
our community will be safer.
However, if you are still concerned about the safety of
these vaccinations, we encouraged you to seek consultation with your
doctor. Click here to speak with our doctors. Our doctors will
be able to assess your medical and allergy history to determine your
eligibility for COVID-19 vaccines.
However, if you still have concerns, you may well get
advice from your consultant.
References
1. “Should heart patients take the COVID-19
vaccine?”. Singapore Heart Foundation. Accessed from
https://www.myheart.org.sg/press-and-media/heart-news/heart-patient-and-covid19-vaccine/
2. “The effects of virus variants on COVID-19
vaccines”. World Health Organization (1 March 2021). Accessed
from
https://www.who.int/news-room/feature-stories/detail/the-effects-of-virus-variants-on-COVID-19-vaccines
3. Merschel, M. “What heart and stroke patients
should know about COVID-19 vaccines”. The American Heart
Association. Accessed from
https://www.heart.org/en/news/2021/01/15/what-heart-and-stroke-patients-should-know-about-COVID-19-vaccines
4. “COVID-19 VACCINATION”. Ministry of
Health Singapore (n.d). Accessed from
https://www.moh.gov.sg/COVID-19/vaccination
5. Will your immune system protect you from
COVID-19 after vaccination?
None of us ever expected that our lives would change indefinitely
when the COVID-19 pandemic took over the entire world by storm. We
are now left to embrace the ‘new normal’ of living.
Something
that still needs getting used to. Some light did come to show early
this year when some pharmaceutical companies begun rolling out the
much-awaited COVID-19 vaccine. Even so, they are increasing the
production of these vaccines as we progress daily.
This is a step in the right direction as it prepares us
to return to normal life by achieving herd immunity – a term
used to describe a huge population that is immune to a virus.
Through
herd immunity, the risk of large-scale outbreaks – like we
have seen over the past year – is significantly reduced1.
However, two important questions remain – can you still get
infected
with COVID-19 after taking the vaccine, and are you eligible for the
vaccine if you have previously tested positive for the virus?
Let’s find out together.
Can those who get vaccinated still contract
COVID-19?
Let us first understand that the COVID-19 vaccines that were
developed have been found to be effective at preventing a COVID-19
infection. However, there is still a minor possibility that you can
contract
COVID-19 despite being vaccinated. Rest assured, that it is a very
slim chance and with vaccination already taking place at break
speed, the risk of COVID-19 infections become even lower.
It’s also important to be aware that the
coronavirus vaccine might not have enough time to provide complete
protection - not that it is ineffective against COVID-19. This is
why mRNA
vaccinations need to be given in two dosages and require
approximately two weeks to fully activate our immune system
response.
So even if an individual has received the vaccination,
practicing cautions in social or physical distancing as well as
basic hygiene is crucial.
Can those who have been previously diagnosed
with COVID-19 be vaccinated?
A person can take the vaccine until the person has recovered from the
acute illness (if the person had symptoms) and they have met
criteria to discontinue isolation. Why? Getting vaccinated can offer
a stronger
and reliable immune system response to a past COVID-19 infection as
compared to the natural immunity developed by the body.
As a matter of fact, those who have recovered from COVID-19
were found to have antibodies that were up to 10 times higher than
vaccinated individuals who did not previously test positive for
COVID-19.
But those with pre-existing immunity experienced systemic side
effects such as fatigue, headache, chills, fever, and muscle or
joint pains with considerably higher frequency This is why those who
fall
in this category are also encouraged to sign-up for vaccination as
soon as possible.
Will life return to normal for those who
have been vaccinated?
Hopefully it will. The most important thing is to do your duty as a good citizen by signing up for the vaccination. However, getting vaccinated against COVID-19 should not be considered a substitute for basic precautionary measures. We should always remember to do our part by practicing good hygiene habits like regular hand-washing, masking up when outdoors, and adhering to social distancing measures. By doing this, we are one step closer to beating the pandemic once and for all.
References
1. “Coronavirus disease (COVID-19): Vaccines”. World
Health Organization (28 October 2020).
Accessed from
https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines
2. “Information about the Pfizer-BioNTech COVID-19
Vaccine”. Centers for Disease Control and Prevention (4 March
2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Pfizer-BioNTech.html
3. “Information about the Moderna COVID-19
Vaccine”. Centers for Disease Control and Prevention (4 March
2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Moderna.html
4. “Key Things to Know About COVID-19
Vaccines”. Centers for Disease Control and Prevention (13
March 2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/keythingstoknow.html
5. Wise, J. “Covid-19: People who have had
infection might only need one dose of mRNA vaccine”. thebmj (2
February 2021).
Accessed from
https://www.bmj.com/content/372/bmj.n308
6. How do the new COVID-19 virus strains affect
me?
Studies have shown that it is natural for any type of virus to evolve
into newer variants. It simply means that viruses can mutate after
some time. This doesn’t mean that they are a new form of a
virus,
but rather a different kind of the same virus.
Best way to describe this is is to think of them as
being part of the same family. Now, these new strains may cause some
changes that are a little different from how we understand the
original
virus to be. While many would panic especially when we keep hearing
about the COVID-19 new variants, its best we first understand how
this mutation works.
It’s true, new strains can either increase or
decrease the risk of a virus being contagious. These strains may
also affect the severity or level of an infection. So, in the case
of
COVID-19, how exactly do new strains affect the level of symptoms?
Does it impact the effectiveness of the different vaccines that are
already available? Let’s take a closer look at how these
happens.
Can a new virus strain cause more severe
COVID-19 symptoms?
Before we dive in a little deeper, it’s important to note that
virus strains exist because of differences in geographic location.
What does that mean, you ask? It means that different countries or
regions may have the same primary virus, but new and different virus
strains may appear in these places simply because of geographical
reasons Let’s look at the virus strain that was originally
detected in the UK for example. This virus strain, also known as
B117, was found to increase the risk of being contagious by up to
50% compared to the original COVID-19 virus. Whoa!
The South African strain - B1351 - on the other hand,
was found to be 50% more contagious than the original COVID-19
virus3. Similarly, the P1 virus strain that was first detected in
Brazil
was found to be up to 2.2 times more contagious than the B117
variant. Pretty intense we would say, but does a higher risk of
being contagious mean that there are more severe COVID-19 symptoms?
Meanwhile, B117 (UK) and B1351 (South Africa) have not
been found to affect the level of COVID-19 symptoms experienced.
However, more data is required to understand the level of COVID-19
symptoms experienced by those infected with the P1 (Brazil) strain.
More recently is the strain discovered out of India
(B.1.617) which has caused global record numbers in daily infections
within the country over the past weeks. It’s still too early
to say if this strain is the cause of rapid spread in India, but
experts are treating it as such. It’s also being called a
“super mutation” that will make its way around to the
rest
of the world. Oh no! This strain has already been detected in
countries like Germany, Belgium and even in the U.K.
This is why it’s important to continue practicing
basic precautionary measures and get vaccinated as soon as possible.
Through this, you are doing your civic duty as a responsible citizen
to prevent further widespread of these new strains.
Can a new virus strain affect the
effectiveness of the different vaccines available?
According to the World Health Organisation (WHO), there is no reason
to believe that these COVID-19 virus strains can cause any vaccine
to be ineffective We can totally breathe easy now! This is because
COVID-19 vaccinations give our bodies some sort of protection by
working with our immune system, which is the body’s natural
defense against viral infections. Through this, our bodies’
natural
defenses cover a wide range of COVID-19 infections, even the new
variants.
On a brighter note, it’s also possible to make
changes to existing vaccines so that they offer better protection
against different COVID-19 virus strains1. This will be especially
important
if data ever shows that these new strains cause the COVID-19
vaccines to be not effective, however there is no such news yet. We
know, what a relief!
What can you do to prevent COVID-19 virus
strains?
Ultimately, it’s important for you to get vaccinated as soon as possible to prevent a COVID-19 infection. And by keeping the spread of the primary virus low, you help to reduce the risk of creating new virus strains in your country or region. Pretty simple, no? At the same time, it’s recommended that you carry on practicing basic measures such as regular hand-washing, masking up, and maintaining social distancing in public areas. By doing this, you can help to reduce the contagiousness of the main COVID-19 virus, whilst reducing the risk of COVID-19 virus strains altogether1. You’ve got this, people!
References
1. “The effects of virus variants on COVID-19 vaccines”.
World Health Organization (01 March 2021).
Accessed from
https://www.who.int/news-room/feature-stories/detail/the-effects-of-virus-variants-on-covid-19-vaccines
2. “Pfizer-BioNTech COVID-19 Vaccine Overview and
Safety”. Centers for Disease Control and Prevention (21 May
2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Pfizer-BioNTech.html
3. CJuan C. Salazar, MD, MPH, FAAP.“What Are the
New COVID-19 Strains, and Do They Infect Kids More Easily?”.
(01 February 2021).
Accessed from
https://www.connecticutchildrens.org/coronavirus/what-is-the-new-b117-strain-of-covid-19-and-does-it-more-easily-infect-kids/
4. Simon Clarke.“Brazil coronavirus variant: what
is it and why is it a concern? An expert explains”. (03 March
2021).
Accessed from
https://theconversation.com/brazil-coronavirus-variant-what-is-it-and-why-is-it-a-concern-an-expert-explains-156234
5. “New COVID variant with 5 mutations identified
in California”. Center for Infectious Disease Research and
Policy (12 February 2021).
Accessed from
https://www.cidrap.umn.edu/news-perspective/2021/02/new-covid-variant-5-mutations-identified-california
6. David Kennedy.“What you need to know about the
new COVID-19 variants”. (16 January 2021).
Accessed from
https://theconversation.com/what-you-need-to-know-about-the-new-covid-19-variants-153366
7. “SARS-CoV-2 Variant Classifications and
Definitions”. Center for Infectious Disease Research and
Policy (25 May 2021).
Accessed from
https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/variant-surveillance/variant-info.html
8. Gayathri Vaidyanathan. “Coronavirus variants
are spreading in India — what scientists know so far”.
(11 May 2021).
Accessed from
https://www.nature.com/articles/d41586-021-01274-7
7. COVID-19 vaccine and orthopedic concerns
A visit to the doctor’s for orthopedic problems (joints, ligaments, tendons, muscles, and nerves) during a pandemic can be an uneasy experience. But it sure can be rewarding if you’re heading there for a COVID-19 shot. Why, you ask? If you have any type of pre-existing health condition, you may be at higher risk of getting COVID-19 than someone else without them. Simple equation!
Therefore, it's important to consider getting vaccinated immediately if you are eligible. But one question could be on your mind: is it safe to give the COVID-19 vaccine to someone who is going for orthopedic surgery? Let’s deep dive together to answer this question, shall we?
Is it safe for those undergoing
orthopedic surgery to take the COVID-19 vaccine?
It's generally safe for you to take the COVID-19 vaccine if you are considered eligible. However, if you are undergoing surgery, you should first consult a doctor before getting vaccinated. Chances are that the doctor will advise you not to take it before surgery.
This is because any side effect from the vaccine may impact the outcome of the surgery. For example, any common side effect such as fever or muscle ache may slow down the rehabilitation or prolong the duration of hospitalization. On the other hand, patients who have experienced physical trauma (fractures, broken or dislocated bones) due to a car accident, fall or sports injury, may be asked upon arrival at the Emergency department if they already have received the COVID-19 vaccination.
Those who have bone or blood-related diseases (bone cancer, osteoporosis, and leukemia) that are severe and can cause terminal illness should also seek consultation with a doctor before getting the COVID-19 vaccine. Better to be safe than sorry, people.
Is it safe to take the COVID-19 vaccine
alongside pain management medicine prior to surgery?
Yes, it is safe for someone who has been given pain management medicine such as steroids for joint pain or inflammation to get the COVID-19 vaccine2. Also, it’s recommended to consult with the clinician in charge for medical advice.
This piece of good news will make no one happier than the elderly. Why the elderly, you may ask? Well, for one, old age can put a person at a bigger risk of injury or developing orthopedic conditions3. For example, arthritis, which requires medicine to manage the pain caused by swollen or tender joints. Ouch!
At the same time, old age can also lower immune system function (your body’s natural defenses) and increase the risk of infectious diseases like COVID-194. This is why it’s important for the elderly to prioritise getting vaccinated, as it can help to protect them against the harmful effects of COVID-19 4.
If you’re not sure about taking the COVID-19 vaccine while on steroid treatment, we encourage you to speak to our orthopedic specialists and come to a decision that works best for you.
Should you get vaccinated prior to
orthopedic surgery?
Yes. But before you do, we recommend that you speak to any of our doctors. They’re best qualified to decide if you are eligible for the COVID-19 vaccine, or if you’re at risk of having health problems due to vaccination. The doctor’s decision to not allow you to take the vaccine relies on things like a weakened immune system, a platelet count that is less than 50,000, and a history of experiencing a severe allergic reaction (also known as anaphylaxis) to venom, certain foods or medication5.
In parting, just remember, It takes a joint (pun intended) effort by everyone to achieve complete immunity within our communities. This starts with prioritising vaccination and other preventive measures such as regular handwashing, masking up in public places, and maintaining social distancing.
References1. Blouhos, K, et al. “Understanding Surgical Risk During
COVID-19 Pandemic: The Rationale Behind the Decisions”.
Frontiers in Surgery.
Accessed from
https://www.frontiersin.org/articles/10.3389/fsurg.2020.00033/full
2. Chakarvarty, K, et al. “Recommendations and
Guidance for Steroid Injection Therapy and COVID-19 Vaccine
Administration from the American Society of Pain and
Neuroscience (ASPN)”.
Dovepress (5 March 2021). Centers for Disease Control and
Prevention (21 May 2021).
Accessed from
https://www.dovepress.com/recommendations-and-guidance-for-steroid-injection-therapy-and-covid-1-peer-reviewed-fulltext-article-JPR
3. Anderson, A. S, MD and Loeser, F. R, MD. “Why is
Osteoarthritis an Age-Related Disease?”. US National
Library of Medicine (24 February 2010).
Accessed from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2818253/
4. “Aging changes in immunity”. MedlinePlus.
Accessed from
https://medlineplus.gov/ency/article/004008.htm
5. “COVID-19 VACCINATION”. Ministry of Health
Singapore (n.d).
Accessed from
https://www.moh.gov.sg/covid-19/vaccination
6. “Thrombocytopenia following Pfizer and Moderna
SARS-CoV-2 vaccination”. The National Center for
Biotechnology Information.
Accessed from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8014568/
Frequently Asked Questions (FAQs) on COVID-19 Vaccines
Covid-19 Vaccine General Information
References
Ministry of Health Malaysia
Academy of Science Malaysia
Last updated on February 2021
For the latest information about COVID-19 Vaccines, please visit
Ministry
of Health Malaysia.
EMERGENCY CONTACT
Gleneagles Hospital Kota Kinabalu
Ambulance / Emergency
+6088 518 911
Gleneagles Hospital Kuala Lumpur
Ambulance / Emergency
+603 4141 3018
Gleneagles Hospital Penang
Ambulance / Emergency
+604 222 9199
Gleneagles Hospital Medini Johor
Ambulance / Emergency
+607 560 1111
Select a hospital