
A gastroenterologist is a medical specialist who focuses on diagnosing and treating diseases of the digestive system, affecting the gastrointestinal tract, including the organs from mouth to anus. They treat conditions such as indigestion, abdominal pain, appendicitis, jaundice, gallstones, lactose intolerance, hepatitis, reflux, ulcers, and hemorrhoids, along with diseases of the oesophagus, stomach, intestines, liver, and pancreas.
We aim to get you back on track to your regular healthy daily life activities. Each treatment option, like these listed below, will be recommended by the top gastroenterologist at Gleneagles Hospital Kuala Lumpur. Our medical team will base these recommendations on your condition, health status, and medical history.
Treatment for Inflammatory Bowel Disease (IBD) may involve various drugs that may be prescribed to reduce inflammation and suppress the immune system that is causing the inflammation, using antibiotics to treat any related infections. Pain relief as well as anti-diarrhoea medication may also be prescribed.
As bowel rest may reduce inflammation, nutrition through feeding tube inserts or via intravenous injections may be recommended for more severe cases.
For drastic measures, surgery to remove diseased parts of the large and/or small intestine may sometimes be required for much more severe cases.
The treatment of Stage 1 and 2 hemorrhoid development may require lifestyle changes and minor medical treatment, which may include:
In many cases, symptoms of haemorrhoids improve or resolve within one to two weeks with these basic measures.
However, if persistent bleeding and painful symptoms occur, more advanced treatments may be required:
For severe or recurring haemorrhoids, surgery might be recommended:
Treatment for Irritable Bowel Syndrome (IBS) typically involves changes in your diet, or completely removing foods that cause bloating, may be recommended by your doctor. Depending on your range of symptoms, fibre supplements, laxative, or diarrheal medication may be prescribed to you.
Depending on your specific symptoms, certain drugs may be prescribed to:
The most effective treatment for this diverticulitis typically involves dietary improvements and, in some cases, antibiotics. Mild cases of diverticulitis infection may only require rest, a liquid diet, stool softeners, and antibiotics. However, surgery may be recommended for more severe cases along with a course of antibiotics and intravenous nutrition.
The primary treatment for colorectal cancer is usually surgery to remove the cancerous tissue. Additionally, your doctor may also recommend chemotherapy as well as radiation therapy before and after successful surgery.
Prescription drugs to neutralise, reduce, and block excessive stomach acid production may be prescribed to treat GERD. Drastic measures include surgery, and procedures such as those listed below may be recommended:
At Gleneagles Hospital Kuala Lumpur, we offer advanced diagnostic and screening services to accurately assess your gastrointestinal health. Our state-of-the-art facilities and comfortable environment ensure a smooth experience throughout the process. Your results will be reviewed by the top gastroenterologists, who will explain and offer the necessary treatment options based on your ailment, lifestyle, and/or risk factors.
Due to the nature of gastrointestinal conditions, a wide variety of symptoms may surface thus a proper diagnosis should first begin with a gastroenterologist questioning family medical history prior to a physical examination. Additional lab tests and imaging may be required such as these below:
Diverticulitis occurs when small pouches (diverticula) in the digestive system become inflamed or infected, typically in the colon.
Common Symptoms of Diverticulitis:
Irritable Bowel Syndrome (IBS) is a digestive disorder that causes discomfort but does not affect bowel tissue or increase colorectal cancer risk.
Common Symptoms of IBS:
Serious Signs to Seek Immediate Treatment:
GERD occurs when stomach acid flows back into the oesophagus, causing irritation and acid reflux.
Common GERD Symptoms:
Nighttime GERD Effects:
IBD includes chronic inflammatory disorders of the digestive tract, such as ulcerative colitis and Crohn’s disease. If left untreated, IBD can lead to severe, life-threatening complications.
Common IBD Symptoms:
IBD symptoms vary based on the severity and location of inflammation. People with IBD may experience remission periods and flare-ups when the disease is active.
Haemorrhoids (or piles) are swollen veins in the lower rectum or anus, which can develop inside the rectum or around the anus.
Common Haemorrhoid Symptoms:
Seek immediate medical help if you experience heavy rectal bleeding, dizziness, or light-headedness.
Colon cancer begins in the large intestine and is part of colorectal cancer, which affects both the colon and rectum. While more common in older adults, colorectal cancer can develop at any age.
Common Symptoms of Colorectal Cancer:
Many individuals may not experience symptoms in the early stages, and symptoms can vary. Regular colorectal cancer screenings are crucial, especially for those with a family history or other risk factors.
The gastrointestinal tract plays a vital role in sustaining health and wellness, starting with water and food. Our digestive process provides us with the foundation to live and carry out daily functions while staying healthy and happy. These few important factors should be taken into consideration to maintain healthy gastrointestinal health:
Are you or a loved one facing any of these gastrointestinal concerns? Our dedicated team of multidisciplinary healthcare professionals are ready for consultation.
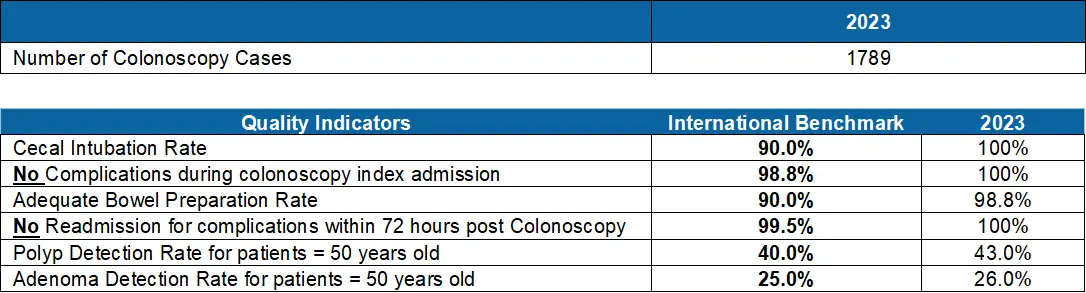
Colonoscopy is a crucial procedure for maintaining digestive health and preventing serious gastrological conditions. At Gleneagles Hospital Kuala Lumpur, the experienced gastroenterologists use advanced techniques to examine the inner lining of the colon and rectum. This procedure helps detect polyps, tumors, and other abnormalities early, allowing for prompt intervention.
We prioritise patient safety and comfort at every step of the process. Our dedicated team ensures a sterile and controlled environment, adhering to stringent safety protocols to minimize any risk of infection or complications. Regular colonoscopies are key to early detection and treatment, providing you with peace of mind and better health outcomes.
At Gleneagles Hospital Kuala Lumpur, achieving international benchmarks for several important quality indicators underscores our dedication to providing top-tier colonoscopy services:
The cecal intubation rate refers to the percentage of colonoscopies reaching and visualizing the whole cecum and its landmark. A complete bowel examination is a prerequisite for thorough and reliable inspection of the mucosa in search of suspicious lesions. A low cecal intubation rate is commonly associated with increased risk of interval colorectal cancer. An incomplete colonoscopy causes an increase in treatment cost and patient comfort as the examination needs to be repeated [1].
Past studies have demonstrated that the quality of bowel preparation affects the cecal intubation rate and detection of adenoma (benign tumours). An inadequate bowel preparation causes increased costs and patient inconvenience as the procedure needs to be rescheduled to a later date. An adequate bowel preparation rate is defined as achieving a Boston Bowel Preparation Rate Scale (BBPS) score of ≥ 6, with each segment of the bowel (ascending, transverse and descending) registering a score of ≥ 2 [1].
The aim of colonoscopy is to reduce the complications and death from colorectal cancer via early detection of tumours at an earlier and more treatable stage and through removal of pre-cancerous adenomas [2]. Adonomas are non-cancerous (benign polyps) that have the potential to develop into cancerous adenomas (adenocarcinoma) [3]. Hence, the Adenoma Detection Rate (ADR) is utilized to gauge the sufficient inspection at screening or diagnostic colonoscopy in patients aged 50 and more. ADR is defined as the proportion of colonoscopies that detect at least one histologically confirmed colorectal adenoma or adenocarcinoma [1,2].
Inclusion factors of Colonoscopy are as follow:
Exclusion factors of Colonoscopy are as follow:
Colonoscopy: Overview of 2023 Data Analysis
Reference
If you or a loved one are experiencing symptoms related to gastrointestinal conditions, don’t wait to seek help. At Gleneagles Hospital Kuala, the experienced gastroenterologists specialise in treating a wide range of digestive disorders, from inflammatory bowel disease (IBD) to colorectal cancer, GERD, IBS, and more. With cutting-edge diagnostic tools like endoscopies, colonoscopy, and CT scans, we ensure accurate diagnoses and personalised treatment plans tailored to your needs.
Maintaining a healthy digestive system is crucial for overall well-being. Our expert team is committed to providing compassionate care and effective treatments to help you return to your daily life with confidence. Book your consultation today and take the first step towards better digestive health at Gleneagles Hospital Kuala Lumpur. Let us help you achieve optimal wellness!
With expertise in treating conditions such as IBD, GERD, colorectal cancer, and liver diseases, the top gastroenterologists at Gleneagles Hospital Kuala Lumpur are here to provide exceptional care for your digestive health. Choose from the experienced specialists, each offering personalised care and advanced treatments tailored to your unique needs. Book a consultation today and meet the best gastroenterologists near you for expert digestive health care.


Wait a minute

Wait a minute