Heart failure occurs when the heart is unable to pump blood effectively, either due to weakness or
stiffness of the heart muscle. It’s a chronic condition that often worsens over time, though it doesn’t
mean the heart has stopped working—it simply requires support to function better.
While heart failure can affect individuals of any age, it is more common among older adults. It is sometimes referred
to as congestive heart failure, although this term is less commonly used today.
Although heart failure cannot typically be cured, symptoms can often be controlled with lifestyle changes and medical
interventions, helping to improve quality of life for many years.
Heart Failure Causes
Heart failure often happens when other conditions have damaged or weakened the heart or if the heart becomes too
stiff. In both instances, the heart does not pump blood efficiently throughout the body. Over time, the heart is not
able to keep up with the body’s normal demand for blood.
Conditions that can lead to heart failure include:
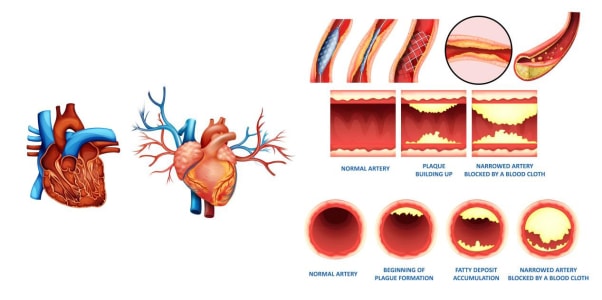
- Coronary heart disease, where the arteries supplying blood to the heart become clogged with fatty substances
(atherosclerosis), which may cause angina or a heart attack.
- High blood pressure can put extra strain on the heart, leading to heart failure over time.
- Conditions affecting the heart muscle (cardiomyopathy) weaken the heart’s ability to pump blood.
- Heart rhythm problems (arrhythmias), such as atrial fibrillation, that affect blood circulation.
- Damage or problems with the heart valves, restricting blood flow.
- Congenital heart disease, birth defects that affect the normal workings of the heart.
Additional factors such as obesity, anaemia, drinking too much alcohol, an overactive thyroid, or high pressure in
the lungs (pulmonary hypertension) can also lead to heart failure. To measure and classify heart failure and its
treatment, an ejection fraction is employed, which helps assess how well the heart pumps blood.
Understanding the Different Types of Heart Failure
Types of heart failure | Description |
Left sided heart failure | Shortness of breath caused by fluid build up in lungs |
Right sided heart failure | Fluid build up in the abdomen causing legs and feet to swell |
Systolic heart failure | Left ventricle cannot contract vigorously indicating a pumping problem |
Diastolic heart failure | Left ventricle cannot fill or relax fully, indicating a filling problem |
Heart Failure Symptoms
The symptoms of heart failure can vary significantly from person to person. They can develop suddenly or gradually
over weeks or months, and they may worsen over time. Recognising these symptoms early can help manage the condition
effectively.
The most common symptoms of heart failure include:
- Breathlessness: This may occur after physical activity or even at rest. It can worsen when
lying down, and you may wake up at night struggling to catch your breath.
- Fatigue: Persistent tiredness and exhaustion, even after rest. Exercise may feel particularly
difficult.
- Swollen Ankles and Legs: This condition is caused by fluid retention, also known as edema. It
may be better in the morning but worsen throughout the day.
- Lightheadedness and Fainting: A feeling of dizziness or sudden fainting spells.
Other symptoms that may occur with heart failure include:
- Persistent Cough
- Difficulty breathing or wheezing sounds when breathing
- Bloated Stomach
- Loss of Appetite
- Weight Gain or Weight Loss
- Confusion
- Fast Heart Rate
- Irregular Heartbeat (Palpitations).
- Depression and Anxiety
Recognising these symptoms early and seeking medical attention is crucial for managing heart failure and improving
quality of life. If you experience any of these symptoms, consult a healthcare provider for an accurate diagnosis
and an appropriate treatment plan.
Heart Failure Diagnosis
If you're experiencing symptoms of heart failure, it's important to consult with your doctor, who will conduct
several checks and a blood test to evaluate your heart’s function.
If the blood test shows a potential issue with your heart, your doctor will refer you to a cardiology specialist team
for further evaluation and tests.
Common Tests for Diagnosing Heart Failure
Several tests may be used to confirm a heart failure diagnosis:
- Blood Tests: These tests check for markers in your blood that may indicate heart failure or
another condition affecting the heart.
- Electrocardiogram (ECG): This ECG test records the electrical activity of your heart to
identify any abnormal rhythms or heart issues.
- Echocardiogram: This ultrasound scan uses sound waves to create images of your heart, helping
doctors assess its size, structure, and function.
- Breathing Tests: These tests, such as spirometry and peak flow tests, evaluate lung function
and check if a lung condition is contributing to your breathlessness.
- Chest X-ray: A chest X-ray can reveal whether your heart is enlarged, if there's fluid in your
lungs (a sign of heart failure), or if another lung issue might be causing your symptoms.
Stages of Heart Failure
Upon diagnosis, your doctor will determine the stage of your heart failure. This helps assess the severity of the
condition and guide treatment decisions. Heart failure is generally classified into four stages:
- Stage 1 – No symptoms during normal physical activity.
- Stage 2 – Comfortable at rest, but symptoms occur with normal physical
activity.
- Stage 3 – Comfortable at rest, but symptoms occur with even minor physical
activity.
- Stage 4 – Unable to perform any physical activity without discomfort, and symptoms may
persist at rest.
Understanding the stage of your heart failure is crucial for your doctor to choose the most appropriate treatment
plan for you.
Heart Failure Treatment
Heart failure requires lifelong management, and while it cannot usually be cured, the right combination of treatments
can significantly help alleviate symptoms and improve quality of life. For most people, treatment of heart failure
requires the right balance of medication and lifestyle changes to alleviate symptoms. In other cases, doctors will
need to investigate any underlying cause or the use of devices to help the heart function properly.
Main Treatments for Heart Failure
- Healthy lifestyle changes
A balanced diet, regular exercise, quitting
smoking, and managing weight are vital for controlling heart failure symptoms and improving heart health.
Participating in an exercise-based cardiac rehabilitation program is often recommended. - Medication
Most people with heart failure require medications to manage
symptoms and slow the condition’s progression. Common medications include ACE inhibitors, angiotensin
receptor blockers (ARBs), beta blockers, diuretics, and others. These medications help relax blood vessels,
lower blood pressure, and improve heart function. Your doctor may adjust the dosage or change medications to
ensure the best results with minimal side effects. - Devices for heart function support
In some cases, medical devices may be
implanted to help control heart rhythm or assist with heart pumping. These include pacemakers, cardiac
resynchronisation therapy (CRT) devices, and implantable cardioverter-defibrillators (ICDs). Devices like CRT-Ds
combine both functions and help those with severe heart failure. - Surgery
In more advanced cases of heart failure, surgery may be
necessary. Options include heart valve surgery, coronary angioplasty or bypass, left ventricular assist devices
(LVADs), or a heart transplant. These procedures help improve blood flow, strengthen heart function, or replace
damaged parts of the heart.
Care Plan for Heart Failure
A care plan tailored to your needs is essential for managing heart failure. This plan will include:
- Management strategies: Detailed plans for ongoing care, including follow-up, rehabilitation,
and access to support services.
- Warning signs: Symptoms to watch for in case the condition worsens.
- Care team contacts: Clear contact information for your care team or specialists.
- Regular reviews: Your doctor should review your care plan every six months to ensure it remains
effective and up-to-date.
Medications for Heart Failure
The treatment regimen often involves multiple medications, which may include:
- ACE inhibitors: Relax blood vessels and help the heart pump blood more easily.
- ARBs: Alternative to ACE inhibitors, used to relax blood vessels without causing a
cough.
- Beta blockers: Slow the heart rate, helping reduce stress on the heart.
- Diuretics: Help remove excess fluid from the body, reducing swelling and
breathlessness.
- Ivabradine and sacubitril valsartan: Specialised drugs for more severe cases of heart
failure.
Each medication has specific benefits, and your doctor will tailor your treatment plan to suit your condition.
Devices for Heart Failure
Some patients may require devices to regulate heart rhythm or assist with pumping. These include:
- Pacemakers: Help regulate a slow heart rate.
- Cardiac resynchronisation therapy (CRT): Corrects asynchronous heart contractions for better
heart efficiency.
- Implantable cardioverter defibrillators (ICD): Prevent dangerous arrhythmias by delivering
shocks if necessary.
- Pulmonary artery pressure sensors: Help monitor blood pressure and assist doctors in managing
treatment adjustments.
Surgical Options for Heart Failure
For severe heart failure cases, surgery may be necessary. Surgical treatments include:
- Heart valve surgery: Replaces or repairs damaged heart valves.
- Coronary angioplasty or bypass: Opens blocked arteries or redirects blood flow to the
heart.
- Left ventricular assist devices (LVADs): Mechanical pumps to assist heart function, sometimes
as a bridge to a heart transplant.
- Heart transplant: A last resort for severe, treatment-resistant heart failure.
5 Key Steps to Managing Heart Failure
1. Record your Weight, Blood Pressure, and Pulse Daily
- If you gain more than 2kg within 48 hours, call your doctor immediately.
- For weight gain of more than 2kg within 48 hours, proceed to a hospital with your medications.
- Swelling in your ankles, legs, and around the waist may indicate fluid retention and could be more noticeable
than weight change.
2. Adhere to Medication Instructions
- Even after feeling better, continue to take your medication as instructed by your doctor.
- Medication seeks to prevent heart failure from progressing, improve symptoms and quality of life.
3. Avoid Caffeine, Alcohol, and Tobacco
- It is highly recommended to stop smoking.
- Consumption of tea and coffee should be in moderate amounts.
- Excessive alcohol consumption is a risk factor for cardiovascular disease and certain types of heart failure.
4. Practice a Low-salt Diet
- Too much sodium in the diet can cause fluids to build up in tissues leading to swelling and breathlessness.
5. Staying Physically Active
- Performing regular physical activities will keep the heart active, gradually increasing stamina, and improve
quality of life.
- Moderate rhythmic exercise such as brisk walking, cycling, and swimming is recommended.
- Activities that require sudden and heavy physical strain should be avoided.
Heart Failure Treatment at Gleneagles Hospital: Expert Care for Your Heart
At Gleneagles Hospital, our team of experienced cardiologists is dedicated to
providing comprehensive heart failure treatment. From diagnosis and medication management to advanced procedures, we
offer personalised care plans tailored to your needs. Trust us to support your heart health with the latest
treatments and medical technology. Book your consultation today and take the first step towards a healthier heart.