

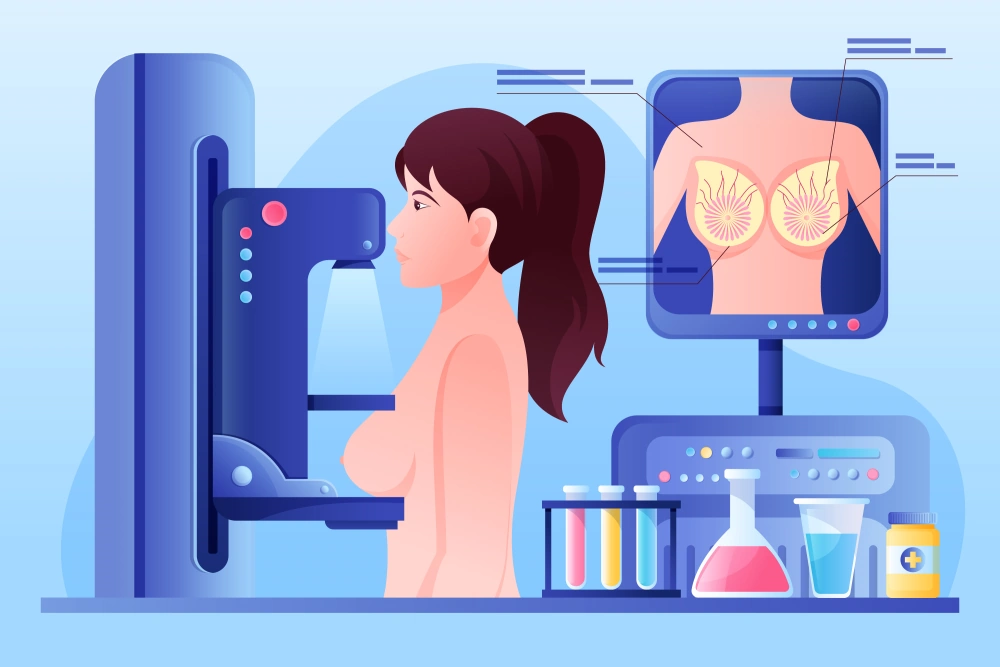
Breast cancer is the most common cancer in women worldwide. Early detection is associated with reduced breast cancer morbidity and mortality. Mammography is a screening and diagnostic tool designed for early breast cancer detection and is considered the gold standard, as it can help to detect breast cancer even before the tumour can be felt in a normal breast examination.
Studies have shown that annual mammography screening in high-risk women beginning at age 40 can lower a woman’s risk of dying from breast cancer and save most lives. Digital breast tomosynthesis (DBT) is a term that is used for 3D mammography. Breast density is associated with reduced mammographic sensitivity and specificity. 3D mammography is found to be superior to conventional 2D mammography for routine breast cancer screening of women with dense breasts.
Studies have shown that 3D has greater accuracy for earlier and easier breast cancer detection. It can improve breast cancer detection by 27-50% and has a lower recall rate by 17-40%, thus fewer women need to return for additional imaging, which will result in decreased patient anxiety and costs.
On a mammogram, both glandular breast tissue and cancers appear white, making it more difficult to identify cancers in dense breasts. In conventional 2D mammograms, the breast is compressed, and images are taken in two views, masses may be obscured by overlapping breast tissue.
View from Different Angles
A 3D mammogram is a significant breakthrough in radiology and helpful for women with dense breast tissue as it can make a better distinction between cancers and overlapping dense glandular breast tissue. In 3D mammography, the breast is compressed, and images of the breast are generated by taking multiple views across the breast in an arc.
The computer software then compiles the views into a three-dimensional reconstruction of the breast to produce a layered 3D image of the breast tissues. The radiologist can view the breast as thin slices, layer by layer and better differentiate cancer from the overlying glandular breast tissue and accurately detect breast tissue abnormalities and breast cancers earlier.
3D mammography is said to decrease the chances of a “false positive” diagnosis and increases the cancer detection rate. Research has shown that a 3D mammogram is up to 40% more sensitive than a 2D mammogram. The main concern for most people, when they undergo certain medical imaging procedures is radiation dose exposure.
Mammogram uses low radiation doses, which are measured in millisieverts (mSv), to get high-quality images. A standard mammogram with two views of each breast contains about 0.4mSv. Radiation dose from a 3D mammogram can range from the same to slightly higher. The amount of radiation dose is slightly higher if a 3D mammogram is done in combination with a 2D mammogram, but the dose is still lower than the United States Food and Drug Administration’s safety limit.
If a synthesized 2D view can be created from the 3D data, then the radiation dose of the 3D mammogram is essentially the same as a conventional 2D mammogram. To put these doses into perspective, the American Cancer Society points out that Americans are normally exposed to an average of 3mSv of radiation each year, just from their natural surroundings.
The dose of radiation used for a screening mammogram of both breasts is about the same amount of radiation a woman would get from her natural surroundings over about seven weeks.
What to Expect
DBT is performed on an outpatient basis though it is not yet available in all Malaysian imaging facilities. If you’re going to a new facility for your 3D mammogram, bring along any prior mammograms or ultrasound images and reports for comparison. Avoid using deodorants, antiperspirants, powders, lotions, creams, or perfumes on your breasts or under your arms.
The metallic particles in some of these products can interfere with the imaging. Wear a two-piece outfit on that day. You will be given a gown and asked to remove any jewelry and clothing from the waist up. Inform your doctor about any breast symptoms, prior surgeries, whether you have a family or personal history of breast cancer, and if there is a possibility you are pregnant.
During this exam, a qualified radiology technologist will position your breast on a special platform on the mammography unit.

Breast Compression
Your breast will be gradually compressed with a compression paddle to even out the breast thickness, spread out overlying breast tissue and minimise blurring so that small abnormalities are less likely to be hidden. Some women with sensitive breasts may experience discomfort. However, note that compression gives better quality images even in DBT examination.
During the examination, the X-ray tube moves from one side of your breast to the other in an arc, capturing multiple images from different angles along the way while your breast remains compressed. Patients are recommended to hold their breath for a few seconds to reduce movement blurring.
The mammogram machine will move above you from one side to another and capture the images. The process is repeated to capture the image of the breast from the other position. The computer-generated images are then analysed by a radiologist. The whole process takes approximately 30 to 40 minutes. After the examination is complete, you may be asked to wait until the radiologist determines all the necessary images have been obtained.
The radiologist interprets the images and sends the report to your primary care or referring physician, who will then discuss the results with you. Breast tomosynthesis should be valuable in both screening mammography and diagnostic mammography. The expected result with this technology is an overall lower recall rate, higher cancer detection rates, a decline in interval cancers, higher positive predictive value for a biopsy recommendation, fewer biopsies, and improved radiologist confidence.
Females who are at risk or show symptoms of breast cancer should consider doing a 3D mammogram, even though the process takes more time. If you are 40 years and above and belong to the high-risk group, do get screened early.
Written by
Dr Vijayalakshmi Krishnapillai
Radiologist
Gleneagles Hospital Kuala Lumpur
This article was first published on 6 December 2020. The full article can be found on The Star*

Wait a minute

Wait a minute