Prepared by Dr Kam Jiyen
Consultant Cardiologist
Gleneagles Medini Hospital
Heart failure is a major health and economic burden in Southeast Asia. Coronary artery disease and hypertension are the main causes of heart failure among adults in this region, accounting for almost 70% of all cases.
Heart failure is a clinical syndrome in which the heart is unable to pump enough blood to meet the metabolic needs of the body. The prevalence of heart failure varies between 3 – 20 per 1000 population, although in persons over the age of 65 years, it could be as high as 100 per 1000 population. Everyday activities such as walking, climbing stairs or carrying groceries can become very difficult as the disease advances.
Left-sided heart failure is more common than right-sided heart failure, and the combination of both is termed congestive heart failure. There are two types of left-sided heart failure:
- Systolic failure, in which the heart loses its ability to contract normally
- Diastolic failure, in which the heart stiffens and loses its ability to relax normally.
There are many reasons why someone may develop heart failure. It can be sudden or it can happen slowly over months or even years. Common causes of heart failure include:
- Coronary artery disease or after a heart attack
- Hypertension
- Cardiomyopathy – a disease of the heart muscle, which can be either inherited or caused by other reasons such as viral infections
- Damaged or diseased heart valves
- Abnormal heart rhythm (arrhythmia)
- Congenital heart conditions – heart problems that one was born with
- Infections
- Some cancer treatments such as chemotherapy
- Excessive alcohol consumption
- Anaemia – lack of oxygen carrying red blood cells in the blood
- Hyperactive thyroid gland disease
The common symptoms of heart failure include reduced physical activities, breathlessness on exertion or upon lying down, leg swelling, chest discomfort, palpitation and sometimes giddiness. These symptoms are caused by reduced forward blood flow to the brain and body as well as back flow of fluid into the lungs and other parts of the body.
To diagnose heart failure, the doctor would take a thorough history and perform physical examination, which include checking the blood pressure, heart rate and rhythm, listening to the heart sounds, and checking for fluid in the lungs, legs or other parts of the body. If heart failure is suspected, further tests are required to confirm the diagnosis.
Some of the common investigations include:
- Blood tests – some specific blood markers are elevated in heart failure or after recent heart attack
- Electrocardiogram (ECG) – to look for abnormal heart rhythm, or clues of underlying coronary artery disease
- Chest X-ray – to check for the heart size and presence of fluid in the lungs
- Echocardiogram (Echo) – this is an ultrasound scan of the heart that is very useful in assessing the heart size and function, as well as heart valve evaluation
Advanced imaging tests are sometimes required to investigate or prognosticate heart failure:
- Cardiovascular Magnetic Resonance Imaging or Cardiac MRI produces amazingly detailed pictures of the heart structures without ionizing radiation. It detects areas of the heart that do not move normally, have poor blood supply or scarred. It provides valuable clues to the cause of heart failure. Stress cardiac MRI with intravenous medication can also be performed to look for potential ischaemia or perfusion defect of the heart muscle.
- Cardiac Computed Tomography Angiogram is a non-invasive test used to check the patency of the coronary arteries.
- Invasive coronary angiogram is sometimes needed for high risk patients especially when coronary revascularisation is indicated.
In general, the survival rate is approximately 50% at 5 years after the diagnosis of heart failure. While there isn't a cure for heart failure at the moment, specific drugs treatments are available to improve symptoms, prevent the condition from getting worse and help to improve the life expectancy.
Some patients with heart failure might benefit from an implantable cardioverter defibrillator (ICD) or a cardiac resynchronisation therapy (CRT). These devices help to prevent sudden cardiac death due to life-threatening arrhythmia and improve the pumping action of the heart. Ventricular assist devices and cardiac transplantation are potential options for selected patients with end stage heart failure.
Alongside taking the medicines as prescribed, making changes to the lifestyle can also help to keep heart failure condition as stable as possible. Such changes may include:
- Weighing regularly – sudden weight gain may suggest too much fluid is building up in the body
- Reduce fluid intake
- Cut down on salt – too much salt in the diet can make body hold on to water
- Stop smoking
- Limit alcohol intake
- Exercise may be helpful to improve overall fitness, but when heart failure is severe, bed rest may be required
If you have signs and symptoms of heart failure, please seek medical attention early. Early treatment saves lives.
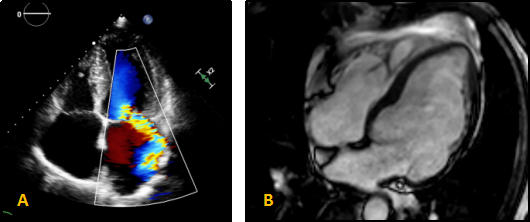
A: Echocardiogram showing abnormal heart chambers and valve leakage
B: Cardiac MRI showing high resolution image of an enlarged heart
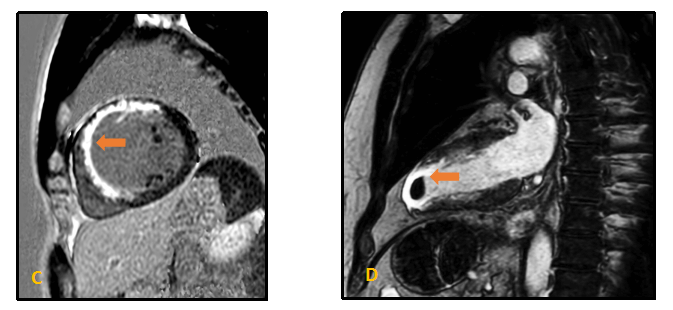
C: Cardiac MRI showing scarred heart muscle in white (arrow) after a heart attack
D: Cardiac MRI showing a clear blood clot (arrow) at the bottom of a heart chamber following a heart attack. This could be possibly missed on an Echocardiogram
 +607 560 1000
+607 560 1000
 +607 560 1111
+607 560 1111



