COVID-19
COVID-19: Symptoms, Preventions & Vaccine
Stay informed and know the facts about COVID-19’s causes, symptoms, diagnosis, preventions and vaccines. Learn about Gleneagles Hospitals’ care and support during this pandemic that include COVID-19 drive-thru screening services, eHealth telemedicine and safety and preparedness plans. At Gleneagles Hospital, your health and safety are our priorities.
COVID-19 : Care and Support
Get information on COVID-19 facts and symptoms, learn how you can reduce the risk of infection, steps you need to take if you have COVID-19 symptoms, download self-care guide and more. It is crucial to learn how to protect your own health and the health of your family members during this pandemic.
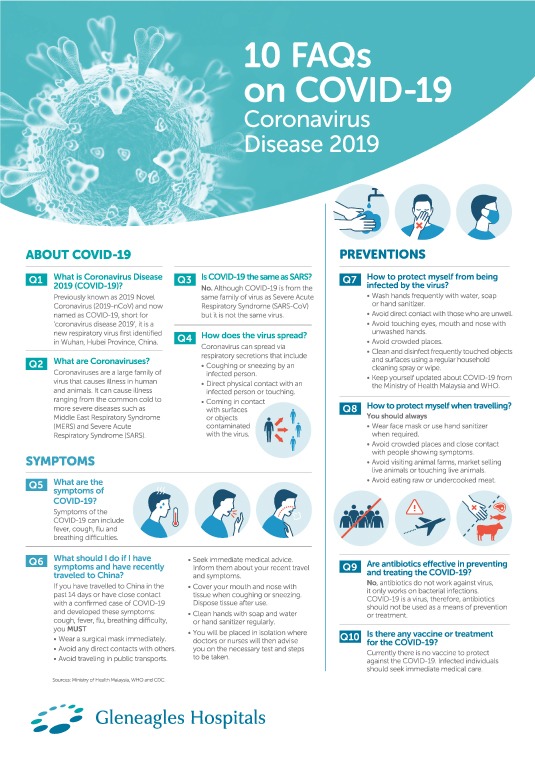
There are a few types of Coronavirus. Coronaviruses are types of virus that typically affect the respiratory tract of mammals, including humans. They are associated with the common cold, pneumonia, and severe acute respiratory syndrome (SARS) and can also affect the gut.
Different types of human coronaviruses vary in the severity of illness they cause and how far they can spread.
Rare but dangerous types include MERS-CoV, which causes Middle East Respiratory Syndrome (MERS), and severe acute respiratory syndrome (SARS-CoV), the coronavirus responsible for SARS.
In December 2019, a novel coronavirus, COVID-19 (previously named ‘2019-nCoV’) has caused an outbreak of respiratory illness. The virus was first detected in Wuhan City, Hubei Province, China. Early on, many of the patients in the outbreak area reportedly had some link to a large seafood and animal market, suggesting animal-to-person spread. However, a growing number of patients reportedly have not had exposure to animal markets, indicating person-to-person spread is occurring.
As of February 2022, COVID-19 has been responsible for over 425 million infections globally, causing over 5.9 million deaths.

Since late 2019, the world has been battling the threat of COVID-19. The spread of the virus and the occurrence of new variants are expected.
In Malaysia, there have been around 3.37 million cases of COVID-19, with 32,634 confirmed deaths from January 3, 2020 to February 27, 2022.
What you need to know about COVID-19
variants
As the virus continues spreading, it also mutates,
creating new variants. Some variants emerge and
disappear while others persist. New variants will
continue to emerge. When new variants
emerge, the virus’s properties, such as how easily
it spreads, the associated disease severity, or the
performance of vaccines also change.
Since late 2020, WHO and researchers have been monitoring all variants. Certain variants may be classified as variants under monitoring (VUM), variants of interest (VOI), variants of concern (VOC), and variants of high consequence. These classifications are based on how easily the variant spreads, how severe the symptoms are, how the variant responds to treatments, and how well vaccines protect against the variant.
Currently designated variants of concern (VOCs) by WHO:
| WHO Label | Earliest documented sample | Date of designation | |||
|---|---|---|---|---|---|
| Alpha | United Kingdom, September 2020 | 18 December 2020 | |||
| Beta | South Africa, May 2020 | 18 December 2020 | |||
| Gamma | Brazil, November 2020 | 11 January 2021 | |||
| Delta | India, October 2020 | VOI: 4 April 2021
VOC: 11 May 2021 | |||
| Omicron | Multiple countries, November 2021 | VUM: 24 November 2021
VOC: 26 November 2021 |
WHO has classified Delta as a VOC as it has been associated with greater transmissibility or detrimental change in COVID-19 epidemiology. The Delta variant is highly contagious; it is at least two times more transmittable. This virus has an infection between 5 and 8, compared to 2.5 and 3 for normal viruses.
Poorly ventilated and crowded indoor spaces are the conditions under which the virus can spread quickly. Fully vaccinated individuals infected with Delta may still spread the virus. However, they seem to have a shorter period of infectivity as the infection rate may be reduced.
What do we know about Omicron?WHO has named variant B.1.1.529 as Omicron and designated it as a VOC on 26 November 2021. This variant has a high number of mutations between 26 and 32 in its spike protein. Since its first detection in South Africa on 24 November 2021, this variant has spread to dozens of countries globally, including the first case in Malaysia on 3 December 2021. It remains unknown whether this variant spreads more easily from person to person than other variants, including Delta. More data are needed to know if infection with the Omicron variant is associated with more severe disease.
What should we do?
Adhering to SOPs and getting vaccinated against
COVID-19 are two effective ways to reduce risk of
contracting COVID-19 or prevent long-term complications
if infected with the virus. At
this point, complete your primary vaccination and
booster dose as immunisation remains the best way to
reduce your risk of severe illness, hospitalisation, and
death from COVID-19.
If you know someone who is confirmed to have COVID-19 and you have been in close contact with them, you should also get tested. Closed contacts of confirmed case were those as below:
- People living in the same household; colleagues working together in the same workspace; classmates in the same classroom environment with a positive COVID-19 case
- Having face-to-face contact with a positive COVID-19 case for more than 15 minutes, less than 1 meter apart, and in an enclosed area
- Being present in an air-conditioned room for more than 2 hours with a positive COVID-19 case although there is no face-to-face contact
- Travelling in the same vehicle (1 or 2 seats apart) with a positive COVID-19 case for more than 15 minutes
The worldwide pandemic has necessitated basic hygiene practices, proper usage of face masks, frequent hand washing, physical distancing, and raised the need for easily accessible COVID-19 tests in Malaysia.
COVID-19 tests in Malaysia are essential in preventing the spread of the pandemic. It can also help patients immediate care.
There are currently two types of COVID-19 tests being used by the health authorities worldwide to detect the virus. The two tests are:
- Molecular tests: Reverse transcription polymerase chain reaction (RT-PCR) tests to detect a virus’ genetic material.
- Antigen tests: Rapid test kit (RTK-Ag) tests to detect specific proteins on the surface of the virus.
To help you understand the function of each test, here’s a helpful comparison of the tests currently available:
| Types of COVID-19 | Tests Molecular Tests (RT-PCR) | Antigen Tests (RTK-Ag) | |||
|---|---|---|---|---|---|
| Also known as | Diagnostic test, viral test, molecular test, nucleic acid test, amplification test (NAAT), RT-PCR test | Rapid Diagnostic Test, usually available as a self-test kit (because the turnaround is often quicker than an RNA test) | |||
| How is the test conducted | Commonly conducted by healthcare professional | • Available as a self-test
kit
• Can also be conducted by a healthcare professional | |||
| How is the sample taken | Nasal or throat swab or saliva | Nasal or throat swab or saliva | |||
| How long does it take for results | Same day (some locations) or may be up to a week | One hour or less | |||
| Is another test needed | This test is highly accurate, usually does not require a second | Positive
– highly accurate
Negative – may need to be confirmed with a molecular test | |||
| What it shows | Diagnoses active coronavirus infection | Diagnoses active coronavirus infection | |||
| What it can’t do | Within the 90 days of someone contracting COVID-19 and getting treated; it won’t be able to test if a person has recovered or not | It won’t be able to rule out active coronavirus infection (antigen tests are more likely to miss an active coronavirus infection, compared to molecular tests) |
The
COVID-19 Neutralising
Antibody Test detects and measures the level of
antibody in your body post completion of the COVID-19
vaccination or a
previous COVID-19 infection.
This test is conducted two weeks post
vaccination to check whether your body responds to the
vaccination and how much of these antibodies are
neutralising antibodies. It also helps
assess potential antibody-association immunity. This
test can also identify individuals with past exposure to
the COVID-19 infection.
As part of our commitment to better serve the community,
Gleneagles Hospitals are providing COVID-19
Drive-Thru Screening Services to ensure your
safety and convenience. The swab test will be performed
through the window of your vehicle.
The PCR Test has a higher sensitivity to
detect COVID-19 compared to the Rapid Test. PCR
technique has an accuracy rate of 99%, whereas many
Rapid Tests in the market has an accuracy
of less than 80%, some as low as 60%.
Book your appointment with
us to get your PCR test via the drive-thru
service at Gleneagles Hospital. You may also contact us
for the COVID-19 Neutralising
Antibody Test two weeks after completion of
second dose of vaccination.
Resources:
- COVIDNOW in Malaysia. Accessed on February 10, 2022 from https://covidnow.moh.gov.my/
- Situasi Terkini COVID-19 di Malaysia. Accessed on February 10, 2022 from https://covid-19.moh.gov.my/terkini
- World Health Organization: Malaysia. Accessed on February 10, 2022 from https://covid19.who.int/region/wpro/country/my
- What You Need to Know About Variants. Accessed on February 10, 2022 from https://www.cdc.gov/coronavirus/2019-ncov/variants/about-variants.html
- Tracking SARS-CoV-2 Variants. Accessed on February 10, 2022 from https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
What is a close contact?
- Shared spaces
- People living in the same household with a positive COVID-19 case
- Colleagues working together in the same workspace with a positive COVID-19 case
- Classmates in the same classroom environment with a positive COVID-19 case
- Close proximity:
- Having face-to-face contact with a positive COVID-19 case for more than 15 minutes, less than 1 meter apart, and in an enclosed area
- Long exposure:
- Being present in an air-conditioned room for more than 2 hours with a positive COVID-19 case although there is no face-to-face contact
- Travelling together:
- Travelling in the same vehicle (1 or 2 seats apart) with a positive COVID-19 case for more than 15 minutes
What to do if you are a close contact to a positive COVID-19 case?
| Vaccination Status | Asymptomatic / Symptomatic | Quarantine Period | Test Requirement |
|---|---|---|---|
| Boosted | Asymptomatic | No quarantine |
|
| Symptomatic | 5 days |
| |
| Fully Vaccinated | Asymptomatic or symptomatic | 5 days |
|
| Partially Vaccinated or Unvaccinated | Asymptomatic or symptomatic | 7 days |
|
- If you test positive, assume you are COVID-19 positive; PCR test is not mandatory
- Follow quarantine SOP for positive COVID-19 case
- During quarantine, if you develop symptoms or they worsen, seek medical attention immediately
- Fully vaccinated close contact individuals who have had COVID-19 infection within the last 60 days do not have to go through quarantine
What to do if you are a positive COVID-19 case?
You will need to update your status and details of close contacts in the MySejahtera app immediately.
| Below 60 years old without comorbidities / Category 1 (no symptoms) / Category 2A (mild symptoms) | Above 60 years old with comorbidities / Category 2B and above (moderate to severe symptoms) / Worsening symptoms | ||
|---|---|---|---|
|
| ||
| Quarantine
period
Fully vaccinated + no symptoms = 7 days Unvaccinated or partially vaccinated + with symptoms = 10 days During quarantine, if your symptoms worsen, seek medical attention immediately.
|
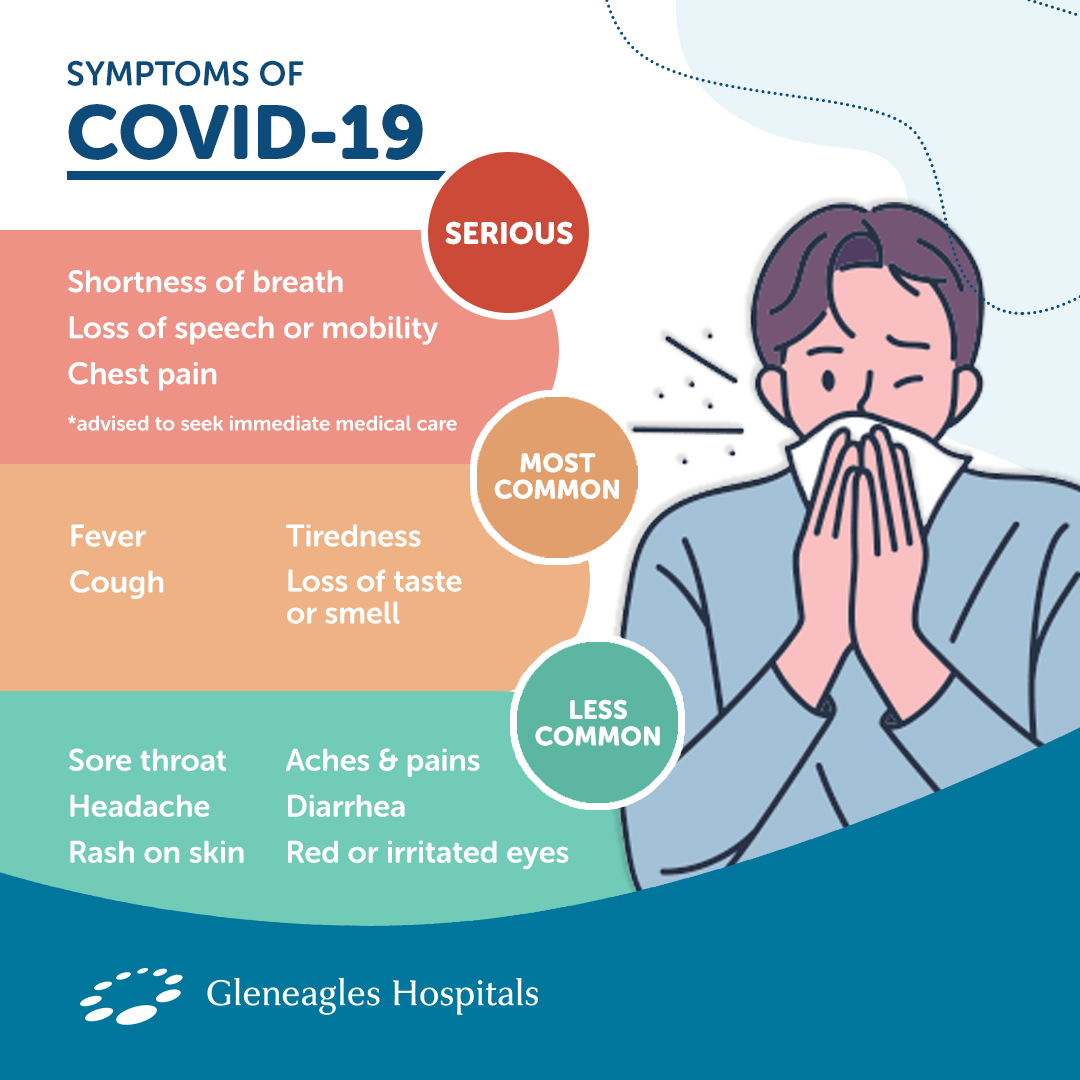
For confirmed COVID-19 infections, reported illnesses have ranged from people with little to no symptoms to people being severely ill. Symptoms may appear 2-14 days after exposure:
Category 1: Asymptomatic
(NEW) Category 2A: Minor symptoms- Sore throat / cold
- Cough
- Loss of sense of taste (but still have appetite)
- Loss of sense of smell
- No fever
- No difficulty breathing
- Diarrhoea twice in 24 hours
- Nausea & vomiting
- Fatigue (but can still do daily activities)
- Muscle aches & pains (but can still do daily activities)
- Fever / onset of fever for more than two days
- Shortness of breath when exerting yourself
- Chest pain
- Loss of appetite
- Fatigue while doing daily activities or after waking up
- Requires walking assistance
- Increasing severity of symptoms (e.g., persistent cough, nausea, diarrhoea, etc.)
- Decreased level of consciousness
- Gradual decrease in urine output over 24 hours
Category 3:
Some breathing issues
Category 4: Requires oxygen
support
Category 5: Needs intubation /
ventilator
Close contacts of positive COVID-19 cases are allowed to quarantine at home (Home Surveillance Order) if you are:
- Below 60 years old
- Have mild or no symptoms (Category 1 and 2A)
- Low-risk individuals (free of co-morbidities and other factors which are likely to worsen the effects of COVID-19 infection)
SOPs for home quarantine
- Dedicated space for isolation: Have a dedicated room to isolate in, preferably with an attached bathroom, especially if you are living with others. Keep the door closed and windows open for ventilation. If the bathroom is shared, it should be cleaned and disinfected after each use.
- Dedicated caregiver: Have a dedicated person to help you get your meals and other necessities sorted out.
- Rest & hydrate: Have plenty of rest, drink lots of fluids, and eat nutritious food to strengthen immune health.
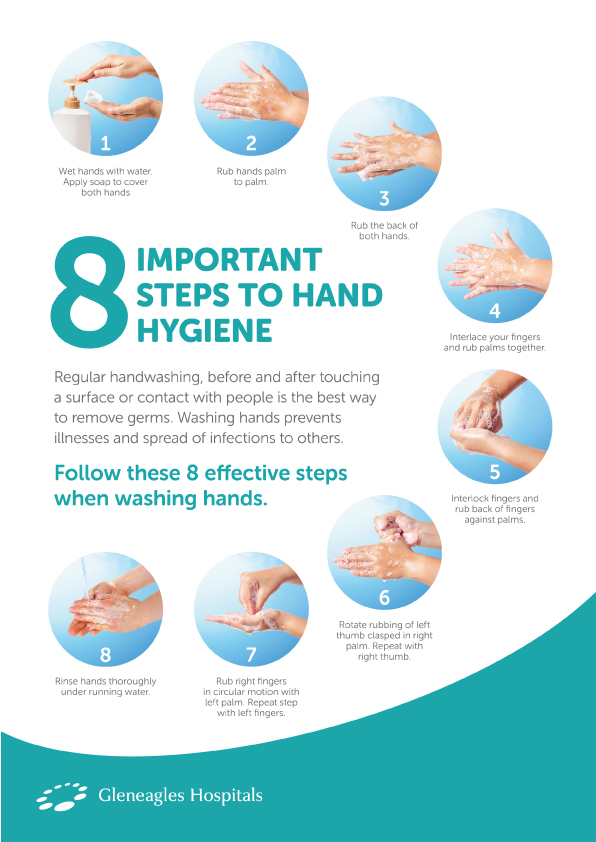
- Personal hygiene: Frequently wash your hands with soap and water and use hand sanitizer. Wear a face mask and observe physical distancing if you need to open your room door to get your meals, packages or garbage disposal. Avoid sharing meals and utensils with others.
- Monitor symptoms: Keep a close eye on your symptoms and report your daily status on MySejahtera. Use a thermometer and oximeter to monitor your temperature and oxygen levels. Contact CAC or hospital immediately if symptoms worsen.
What to avoid during home quarantine
- Have visitors over: Avoid inviting or allowing visitors to your house.
- Go out: Do stay in your room and avoid leaving our house to buy food, medication, etc. Do get your dedicated caregiver to help you with the necessary tasks.
- Self-medicate: Avoid taking advice from social media, always contact a healthcare professional
The home quarantine SOPs are also relevant to those who are:
- Waiting to take a COVID-19 test
- Waiting for COVID-19 test result
- Waiting to be admitted to hospital
- Waiting for further instructions from health authorities
- Unwell and living in a shared space
The COVID-19 virus can incubate in humans from 5 to 14 days, but the result of having COVID-19 can have longer term consequences than most people realise. Where symptoms last beyond the 4-to-12-week time frame, it is referred to as ‘long COVID’, ‘long-haul COVID’, or ‘post-COVID syndrome’.
Common Signs and Symptoms
Ear, Nose, and Throat (ENT)
ENT symptoms have always been a hallmark of the COVID-19 virus. This still remains the case, and while the symptoms tend to overlap with the common flu, they tend to be more pronounced and chronic in how they affect the individual. Those afflicted can expect to experience a range of symptoms including tinnitus (ringing in the ear), earache, sore throat, loss of taste and/or smell.
Respiratory
The respiratory element of the COVID-19 virus is a common occurrence in patients. This often results in breathing difficulties, and is often coupled with a persistent cough that does not abate. In severe cases, regular oxygen use may be necessary.
Cardiovascular
As respiratory factors have an effect on the cardiovascular system, long haul patients can expect to experience chest tightness, chest pain, and palpitations (the sensation of your heart pounding or racing). These are often more prevalent in patients with pre-existing conditions which are diabetic, respiratory or cardiovascular in nature.
Gastrointestinal
While nausea and diarrhea are common symptoms present at the onset of the COVID-19 infection, they may carry on in a mild to severe combination of abdominal pain, reduced appetite, and/or resulting anorexia.
Neurological
As the long-haul symptoms take their toll on the body, neurological symptoms (associated with the brain) may set in as well. This may be mild or severe and include cognitive impairment (brain fog, loss of concentration, memory loss), headache, sleep disturbance, peripheral neuropathy symptoms (loss of feeling in extremities), dizziness, and/or delirium.
Muscular
Further associated with long-term illness, patients may experience muscular symptoms such as joint pain, muscle pain, or a general feeling of lethargy for the duration of the illness, and post-recovery. This may occur in specific parts of the body, or affect the body in a more generalised manner.
Dermatological
Long haul COVID-19 may result in chronic or permanent skin problems such as skin rashes and hives. There may also be swelling in the fingers and toes which is tender to the touch and appears similar to bruising. Other uncomfortable symptoms include sores on the lips and mouth. Both of these latter conditions often heal over time once the patient recovers.
Managing Your Symptoms
Should you suffer from ‘long-haul
COVID’, ensure that you eat well and drink plenty
of water during this time to aid in your recovery.
Paracetamol (up to 1000 mg every 6 hours),
antihistamines (up to 3 times a day), and cough syrup
(up to 3 times a day) are possible methods of treating
the symptoms to ease your discomfort. However, do
consult with your doctor prior to
consuming any new medication.
From June 2020 to December 2021, the MIS-C Malaysia Study Group found that a total of 174 cases were identified in Malaysia and 57% of the total cases were among children aged 5-11 years old.
What is Multi-System Inflammatory Syndrome in Children (MIS-C)?MIS-C is a life-threatening complication caused by COVID-19 infection in children. This condition causes organs to become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, and gastrointestinal organs. So far, seven deaths have been recorded as a result of MIS-C.
What are the symptoms of MIS-C?
- Fever for more than 4 days
- Abnormal physical weakness or lack of energy
- Loss of sense of taste / smell
- Extreme fatigue
- Breathing difficulty
- Coughing
- Nauseous
- Diarrhoea
- Rashes
- Swollen lymph nodes
- Neck pain
- Red and cracked lips
- Bloodshot eyes / conjunctivitis
- Shock syndrome
- Needs Veno-arterial Extracorporeal Membrane
- Oxygenation (VA-ECMO)
- Coronary dilation
- Pericarditis
Parents and guardians should get the COVID-19 vaccines for their children aged 5-11 years old to protect them from COVID-19 and its related medical complications including MIS-C.
The Cominarty for children vaccine uses a new and safe formulation and dosage that is appropriate for children in that age range.
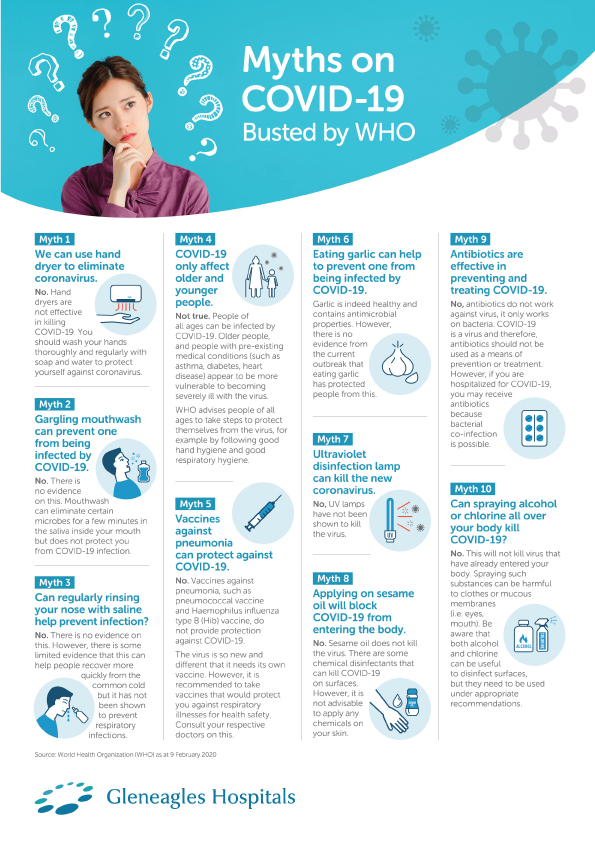
It is important to protect yourself and those around you by taking the right precautionary measures to reduce the risk of coronavirus infection.
- Get tested if unwell: If you are showing COVID-19 symptoms such as fever, cough, sore throat, etc., do a self-test immediately
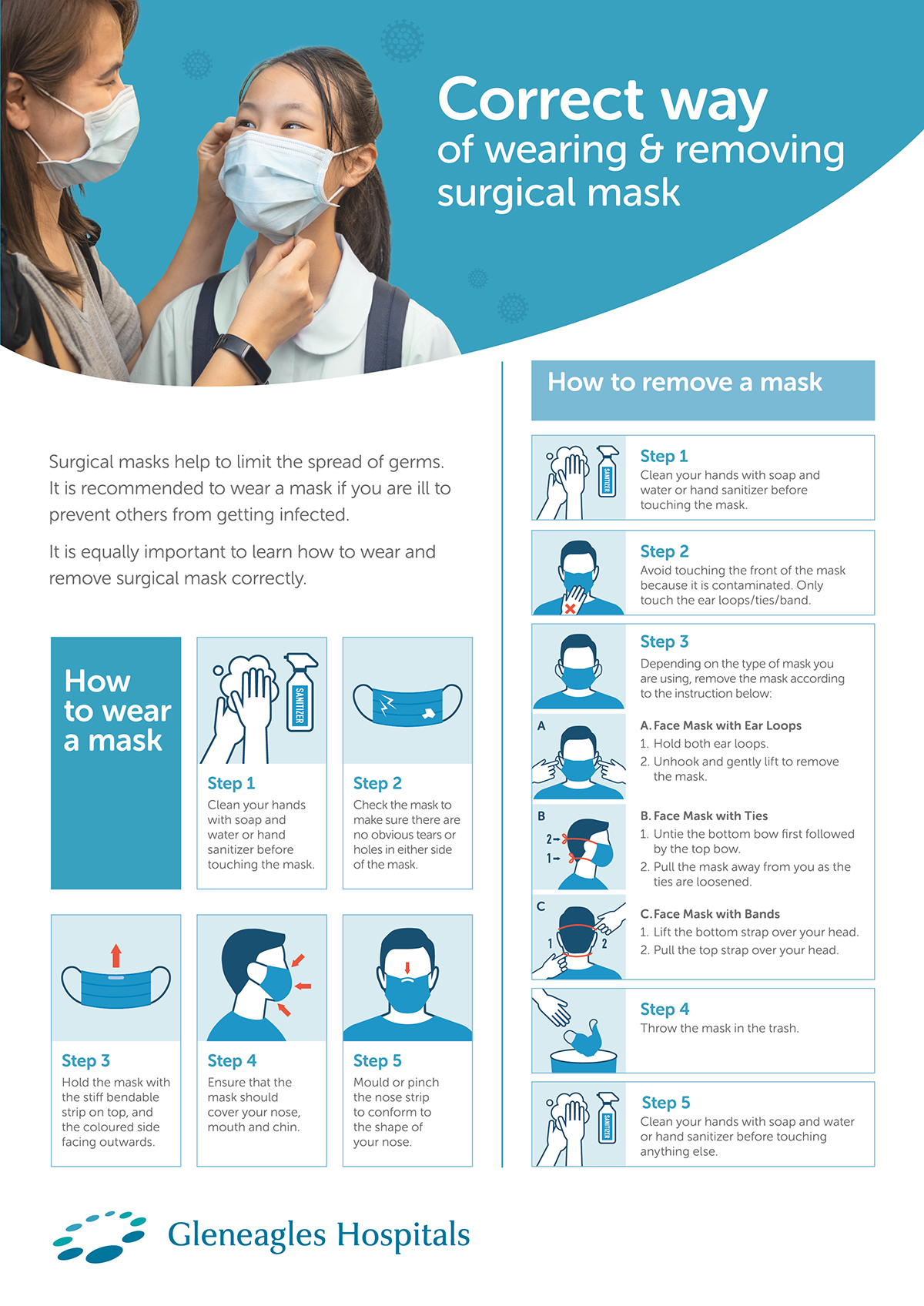
- Always wear protective face mask: When you are going out of your house and meeting with others, always wear a face mask properly
- Keep your hands clean: Wash your hands often with water and soap or clean them with 60% - 70% alcohol-based gel, foam or liquid sanitizer
- Physical distancing: Practice adequate physical distancing (1-2 meters apart)
- Avoid the 3Cs: Stay away from Closed areas, Crowded places, and Close interactions
- Test before gathering: Do an RTK test before attending gatherings with other people
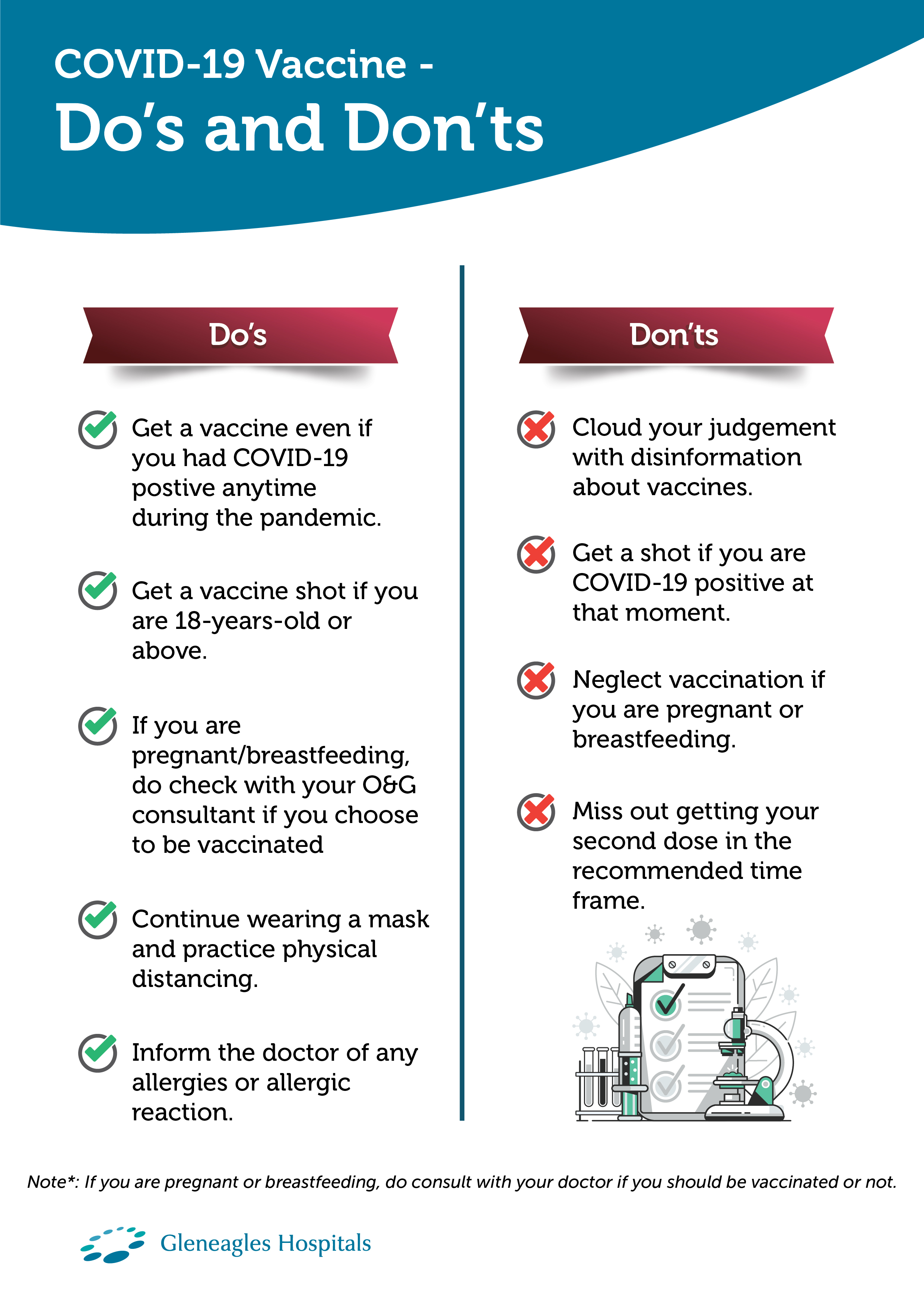
- Get vaccinated: Studies show that vaccination provides the best protection against COVID-19 infections, in particular severe illness and death. Ensure that you and your family are fully vaccinated. Take your booster doses when you become eligible for them. Consider enrolling your children for vaccination once it is available to them.
Unvaccinated people are 9x more likely to be infected and 62x more likely to die from COVID-19 infection.
For the latest information about COVID-19, please visit
Ministry
of Health
Malaysia.
Source: Ministry of Health Malaysia, WHO, CDC
- https://covid-19.moh.gov.my/garis-panduan/garis-panduan-kkm/ANNEX_2e_CLINICAL_MANAGEMENT_OF_CONFIRMED_COVID-19_CASE_IN_ADULT_AND_PAEDIATRIC_13082021.pdf
- https://covid-19.moh.gov.my/garis-panduan/garis-panduan-kkm/ANNEX_2_Management_of_Suspected_Probable_and_Confirmed_COVID19_04062021.pdf
- https://covid-19.moh.gov.my/garis-panduan/pemantauan-kendiri-kes-positif-covid-19-di-rumah
- https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
- https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- https://covid-19.moh.gov.my/semasa-kkm/2021/06/long-covid-post-covid-syndrome
For the latest information about COVID-19, please visit
Ministry
of Health
Malaysia.
Source: Ministry of Health Malaysia, WHO, CDC
- https://covid-19.moh.gov.my/garis-panduan/garis-panduan-kkm/ANNEX_2e_CLINICAL_MANAGEMENT_OF_CONFIRMED_COVID-19_CASE_IN_ADULT_AND_PAEDIATRIC_13082021.pdf
- https://covid-19.moh.gov.my/garis-panduan/garis-panduan-kkm/ANNEX_2_Management_of_Suspected_Probable_and_Confirmed_COVID19_04062021.pdf
- https://covid-19.moh.gov.my/garis-panduan/pemantauan-kendiri-kes-positif-covid-19-di-rumah
- https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
- https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- https://covid-19.moh.gov.my/semasa-kkm/2021/06/long-covid-post-covid-syndrome